

Background: A main concern for juvenile idiopathic arthritis (JIA) patients is frequent non-adherence to treatment which may affect prognosis, delayed resolution of disease and increased complication rates.[1] Possible reasons for non-adherence include irrational fears about the adverse events of prescribed drugs and lack of understanding of disease progression.[1] In order to bridge this knowledge gap of patients and caregivers, the Specialized Pharmacist Education for Children with Idiopathic Arthritis & Laypersons (SPECIAL) program was implemented for all newly diagnosed patients.
Objectives: To evaluate the effectiveness of the SPECIAL program.
Methods: Standardized content for the counselling included information about JIA, its management and drug monographs. These monographs detailed pediatric specific adverse effects and management. This material was provided to patients at the end of the session as a booklet in English or Mandarin. Only caregivers who attended the full counselling were invited to participate in the study.
Self-administered questionnaire QA was compiled by rheumatologists, nurses and a pharmacist and covered information of the counselling content and common misconceptions. Questionnaire QB had the same questions as QA in a different order to assess post-counselling knowledge. Correct responses scored 1, incorrect responses scored -1, “Not sure” responses scored zero, score range -10 to 10. QB included a survey on satisfaction of the service, score range 5-35. The questionnaire was pre-tested in 5 caregivers and patients. Minor editing was done before giving the questionnaires subsequently.
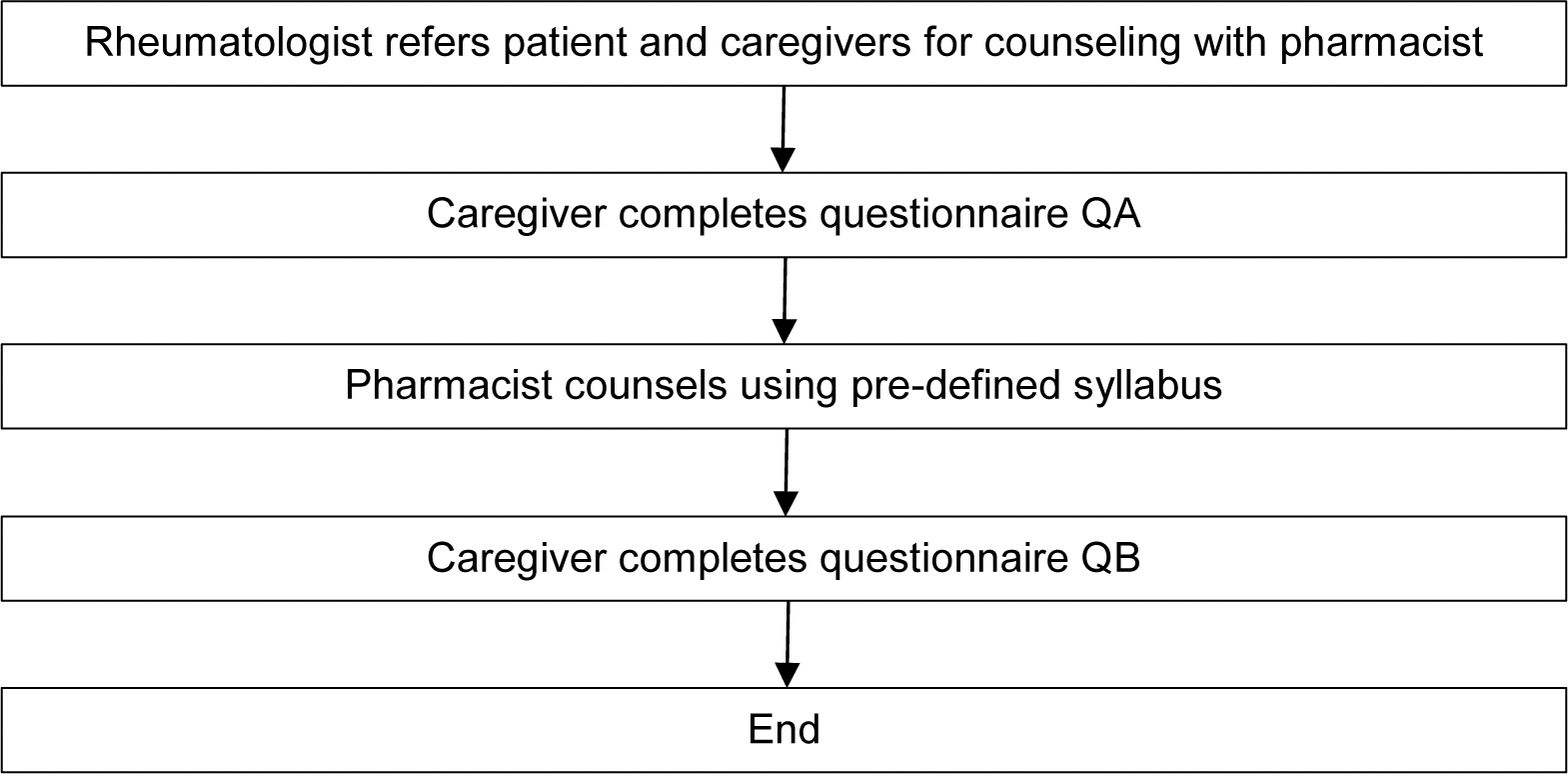
After assessment by a pediatric rheumatologist, newly diagnosed JIA patients and caregivers were directed to receive the counselling by a trained pharmacist in English or Mandarin. Caregivers first completed QA. Then the pharmacist proceeded with the counselling and they were allowed to ask questions. After the session, caregivers completed QB (Figure 1). This study was exempted from review by SingHealth institutional review board.
Flow for the study
Pre and post counselling knowledge and patient satisfaction score, median and range of scores were reported and were compared using Wilcoxon signed-rank test and α<0.05 was considered statistically significant.
Results: From 1 Jan 2020 to 30 Nov 2023, 42 counselling sessions were conducted which included 18 full and 24 drug counselling spanning over 46 hours. A total of 14 surveys from caregivers were collected, 4 caregivers declined participation. Median age of caregivers was 43 (range 34-57) years. Most caregivers were Chinese (10/14), and most (9/14) had at least tertiary education. Caregivers’ knowledge improved significantly from median score 5 (range 3-10) pre-counselling to median score 10 (range 6-10) post-counselling (p=0.006). There was no significant change in caregivers’ confidence in managing the condition after counselling (p=0.058). Question with the lowest pre-counselling score was the need for regular eye checks. Median satisfaction score was 32 (range 20-35).
Conclusion: The SPECIAL program significantly increased caregivers’ knowledge of JIA and its management and was also well received by caregivers. This program also saved 46 hours of clinic time which could be better utilized by physicians to review other more complex cases. Future sessions should include emphasis of questions with lowest pre-counselling scores and expanded to other rheumatologic conditions. The clinical impact of this program on patient adherence and clinical outcome should be explored subsequently.
REFERENCES: [1] Favier LA, Taylor J, Loiselle Rich K, Jones KB, Vora SS, Harris JG, Gottlieb BS, Robbins L, Lai JT, Lee T, Kohlheim M, Gill J, Bouslaugh L, Young A, Griffin N, Morgan EM, Modi AC. Barriers to Adherence in Juvenile Idiopathic Arthritis: A Multicenter Collaborative Experience and Preliminary Results. J Rheumatol. 2018 May;45(5):690-696. doi: 10.3899/jrheum.171087.
Acknowledgements: NIL.
Disclosure of Interests: None declared.