

Background: Obesity has been linked to an increased risk of chronic musculoskeletal pain. This may be attributed to metabolic effects and/or mechanical stress on weight-bearing sites. Although most research originates from adults, both obesity and maladaptive pain have paediatric roots, and chronic musculoskeletal pain may require early prevention.
Objectives: We aimed to quantify the prospective association between childhood adiposity trajectories and pain outcomes in adolescent boys and girls.
Methods: We used data from Generation 21, a population-based birth cohort established in 2005/6 in Portugal. Children were recruited at birth and followed-up through physical examinations and interviews at ages 4, 7, 10 and 13 years.
As exposures we used two adiposity indices: fat mass percentage (FM%), obtained through tetrapolar bioimpedance, and body mass index z-scores (z-BMI), both measured at 4, 7, 10 and 13 years of age. Individual adiposity trajectories over time were extracted from separate mixed-effects polynomial trend models for each adiposity measure and each sex. We fit models up to the quadratic term, selected based on goodness of fit indicators, allowing for random terms for intercept (initial adiposity), linear slope (rate of change) and quadratic slope (acceleration).
We used binary logistic regression models to quantify the associations between adiposity trajectories and two pain outcomes: chronic (duration of 3+ months) and multisite pain (2+ sites). Multinomial regression was used to assess the association between adiposity trajectories and different pain sites (musculoskeletal, head, abdomen/pelvis, and other). Models were adjusted for pubertal development measured through Tanner pubic hair stage at age 13 and stratified by sex. Results indicate how the odds of experiencing pain outcomes change with each standard deviation increase in each of the trajectory terms (initial value, rate of change and acceleration).
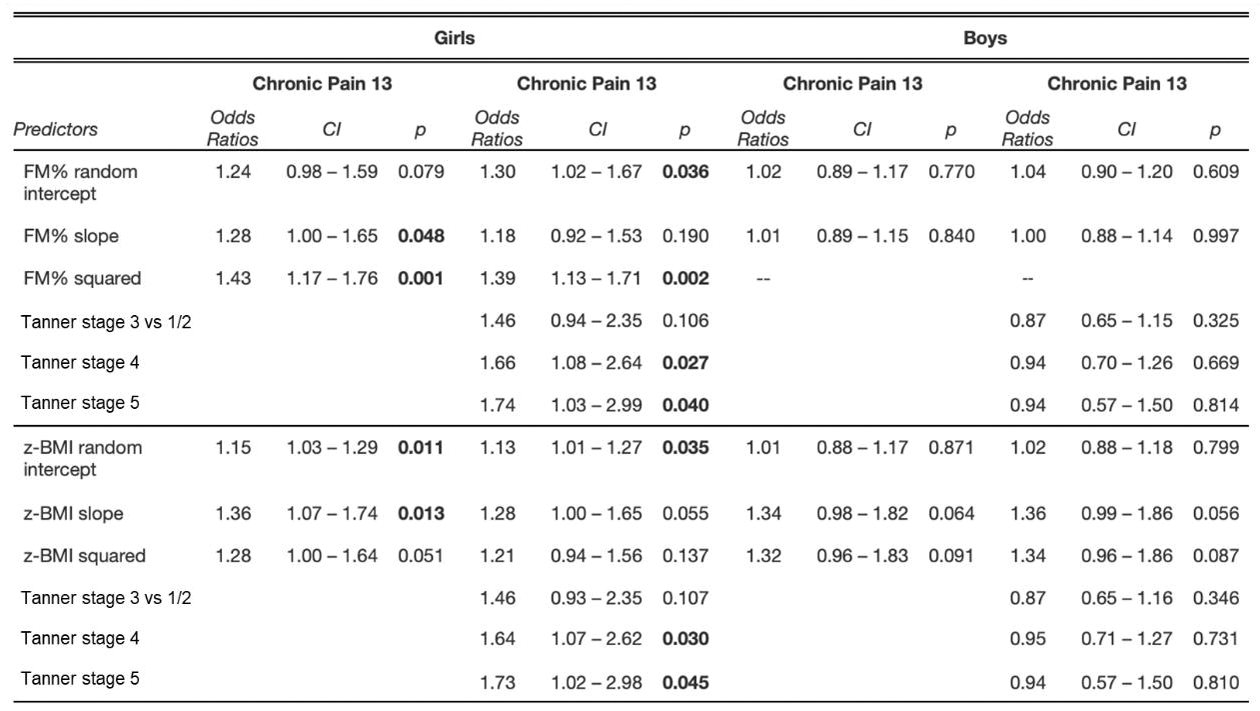
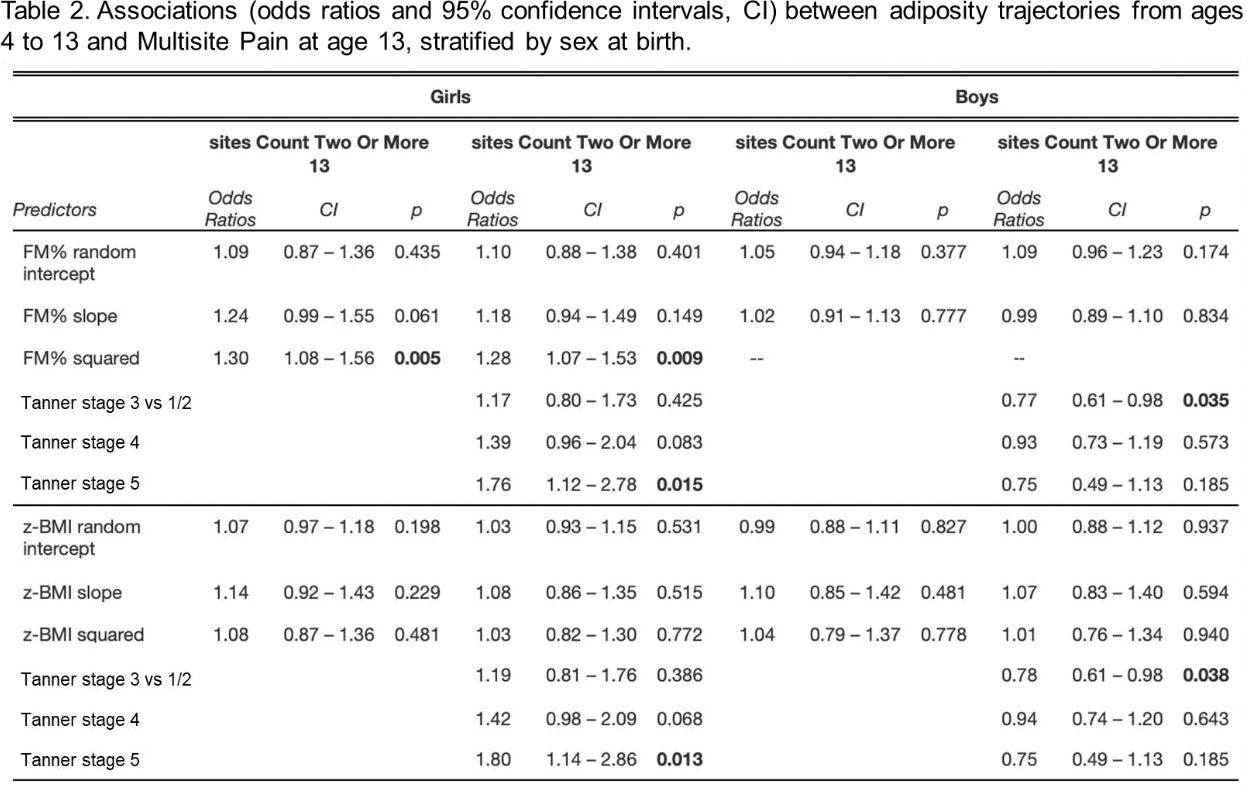
Results: We included 2209 girls and 2354 boys with complete data from ages 4 to 13. Among girls, we observed clear associations between trajectories of adiposity and chronic and multisite pain at age 13 (Tables 1 and 2). After adjusting for pubertal stage, higher initial value and acceleration of FM% accrual were associated with increased odds of reporting chronic pain at age 13 (odds ratio [OR] 1.30, 95% confidence interval [CI] 1.02, 1.67; OR 1.39, 95% CI 1.13, 1.71). A greater FM% acceleration was also associated with increased odds of reporting pain in multiple sites at age 13 (OR 1.28, 95% CI 1.07, 1.53). BMI trajectories were associated with chronic pain at age 13 in girls, particularly the intercept (OR 1.13, 95% CI 1.01, 1.27), and slope (OR 1.28, 95% CI 1.00, 1.65). Furthermore, multinomial regression models showed that, in girls, chronic pain in musculoskeletal sites was significantly associated with FM% initial value (OR 1.44, 95% IC 1.01, 2.06) and acceleration (OR 1.54, 95% IC 1.13, 2.09), as well as z-BMI initial value (OR 1.17 95% IC 1.00, 1.37). In contrast, we did not find any relevant associations among boys.
Conclusion: Among girls, faster adiposity gain from ages 4 to 13 was associated with both chronic and multisite pain in early adolescence, in particular at musculoskeletal pain sites. No such associations were found in boys. Our findings support an early sex-specific association between adiposity trajectories and maladaptive pain, consistent with a metabolic effect of fat on pain report.
REFERENCES: NIL. Table 1. Associations (odds ratios and 95% confidence intervals, CI) between adiposity trajectories from ages 4 to 13 and Chronic Pain at age 13, stratified by sex at birth
Acknowledgements: This work was supported by a research grant from FOREUM Foundation for Research in Rheumatology (Career Research Grant). The cohort study is supported by FCT - Fundação para a Ciência e Tecnologia, I.P. through the projects with references UIDB/04750/2020 and LA/P/0064/2020 and DOI identifiers
Disclosure of Interests: None declared.