

Background: Juvenile idiopathic arthritis (JIA) represents the most closely associated inflammatory disease with pediatric uveitis, being its most common extra-articular manifestation (10-30%). The majority of JIA patients will develop uveitis within the first four years from the onset of arthritis. Screening guidelines based on risk factors are recommended. Evidence supports the early introduction of systemic immunosuppressive drugs, such as methotrexate and adalimumab, to control intraocular inflammation and prevent associated complications.
Objectives: The study objectives are to analyze factors associated with the development of uveitis.
Methods: We conducted a retrospective, longitudinal, multicenter study. Patients with non-infectious uveitis associated with JIA were selected from a multicenter cohort. The time of onset of uveitis was analyzed, as well as the presence of associated complications. Known risk factors (age, gender, antinuclear antibodies (ANAs), JIA subgroup according to the ILAR classification) have been examined. Furthermore, the treatment (systemic immunosuppressive drugs) received by patients with JIA when they developed uveitis was evaluated, along with its duration.
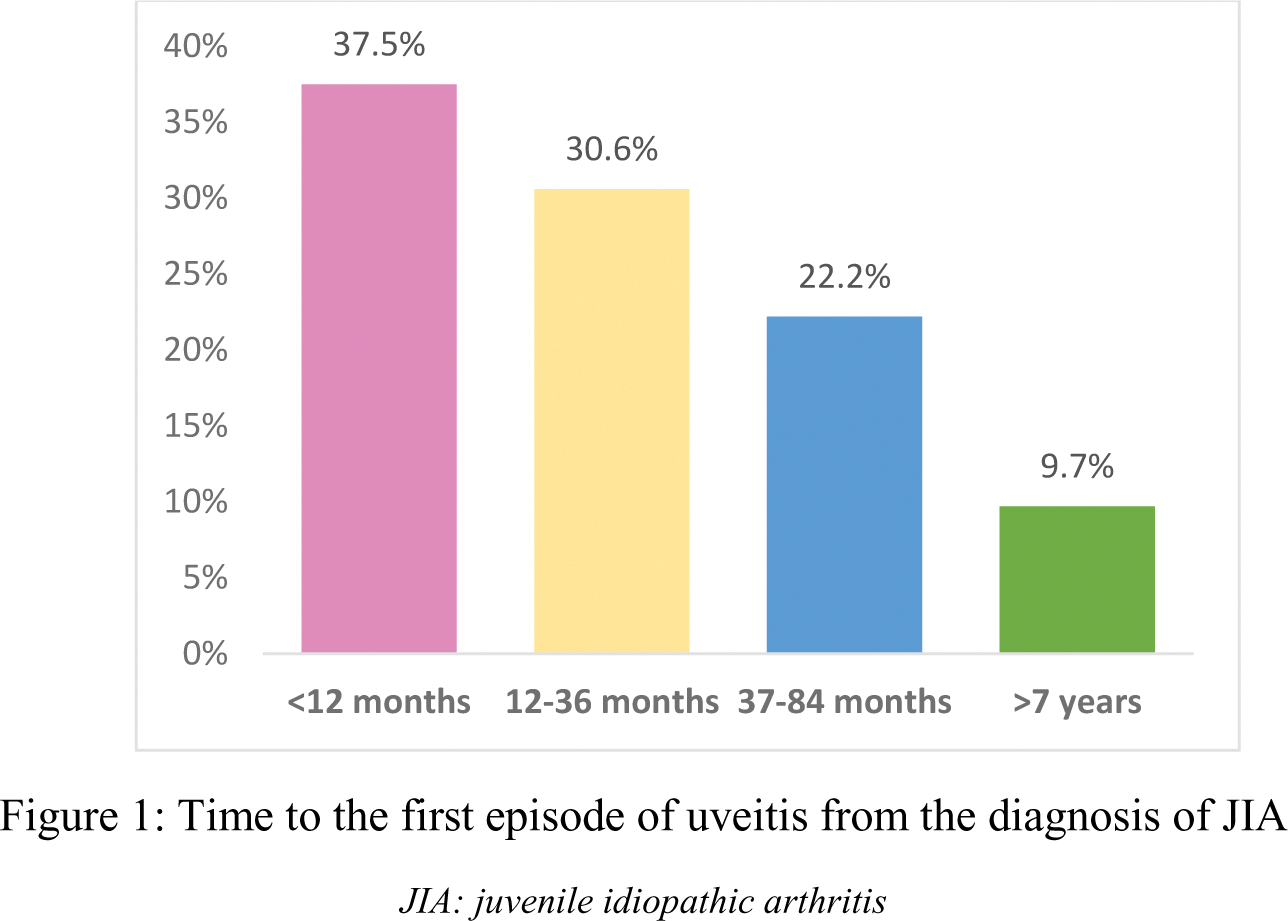
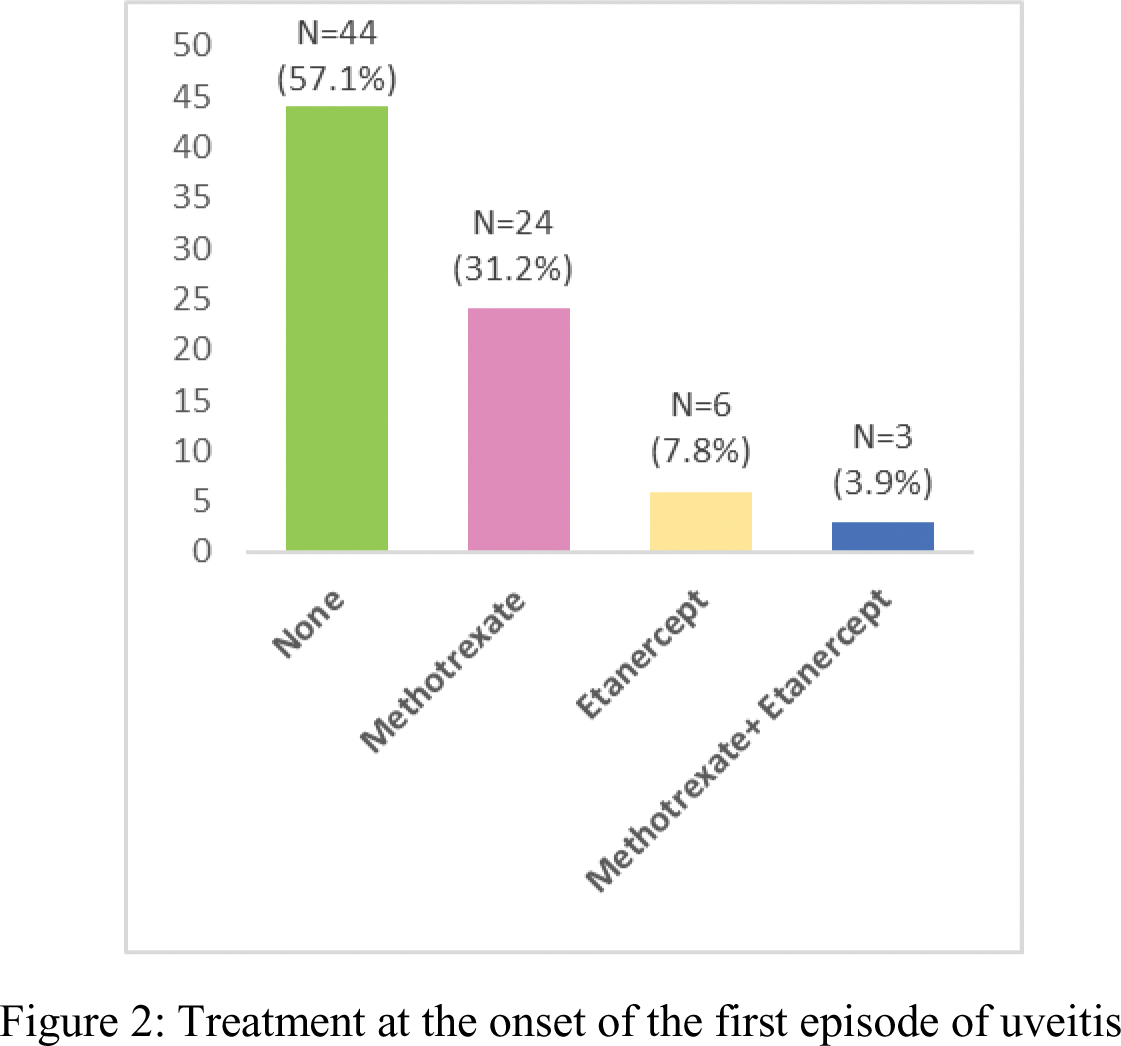
Results: Out of a total of 404 patients with JIA, we included 77 (19%) who had a diagnosis of uveitis (75% anterior chronic uveitis), of whom 18.2% experienced ophthalmological sequelae. 72 had arthritis preceding (54.5% persistent oligoarticular JIA), mostly girls (73%), with positive ANAs (61%). 37.5% developed uveitis within the first 12 months from diagnosis (Figure 1) with a median time to uveitis of 1.6 years. 74 patients received methotrexate, with a median duration of 3 years. In the first uveitis flare, 24 patients were being treated with methotrexate, and 6 with etanercept (Figure 2). Among patients who discontinued methotrexate before the onset of uveitis, the median time until its appearance was 1.7 years.
Conclusion: Our study confirms that uveitis develops in the early years following the diagnosis of JIA, but the risk of occurrence persists throughout the course of the disease. More than half of the patients developed uveitis while not receiving systemic treatment. We observed that those receiving methotrexate as monotherapy had a higher frequency of uveitis compared to other treatments.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.