

Background: Juvenile idiopathic arthritis is classified differently, with enthesitis-related arthritis (ERA) and polyarticular arthritis being the most frequent in adults [1].
Objectives: The purpose of this study was to examine the clinical features and functional status of patients with ERA and polyarticular arthritis in an adult cohort on biological disease-modifying antirheumatic drugs (bDMARDs).
Methods: The HUR-BIO database, a single-center database that records patients receiving bDMARDs prospectively, was founded in 2005. HUR-BIO has documented three disease groups: spondyloarthritis (SpA) (3448 patients), rheumatoid arthritis (RA) (2365 patients), and psoriatic arthritis (PsA) (634 patients). Out of 6447 cases, 167 (2.6%) were diagnosed before the age of sixteen. These patients were identified as having juvenile idiopathic arthritis. According to the ILAR classification criteria, 147 patients were defined as ERA and polyarticular (RF positive or negative). The following data was recorded: the demographics of these two groups; the ages at which the bDMARDs were started; the history of bDMARD and steroid use; the disease activity both prior to bDMARD use and the last follow-up (DAS-28); the functional status (HAQ-DI); the rates at which the bDMARDs were continued; the presence of changes between bDMARDs; the presence of Familial Mediterranean Fever (FMF); and the presence of the hip/knee replacement.
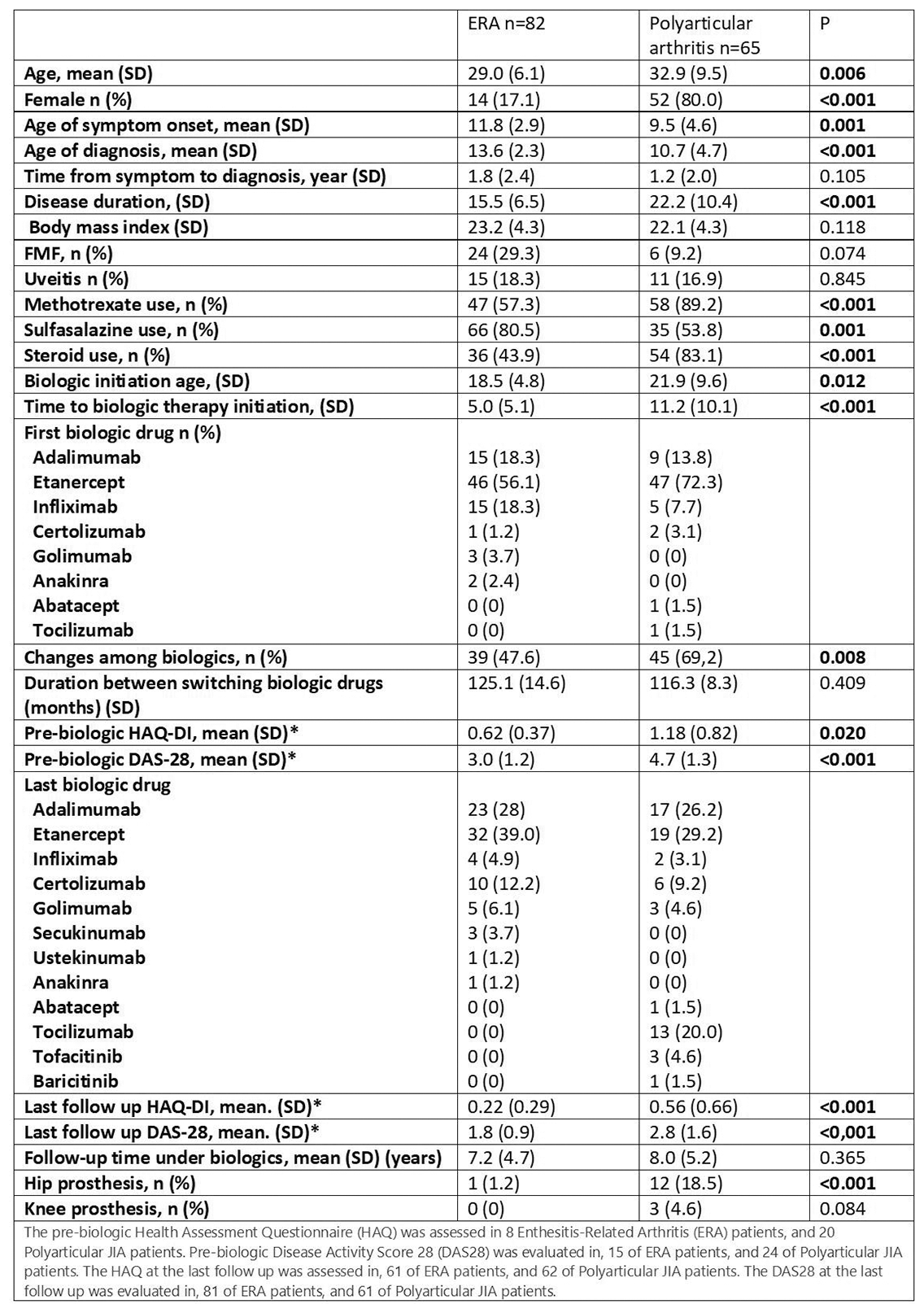
Results: The study included 82 ERA (17.1% female) and 65 polyarticular arthritis patients (80.0% female). Among patients with polyarthritis, RF was positive in 26 (40.0%) cases. In ERA patients, symptoms appear at the age of two and are diagnosed three years later. Patients with ERA used sulfasalazine more frequently, while those with polyarthritis used methotrexate and steroids. In ERA patients, the time to bDMARD was significantly shorter than polyarthritis (5.0±5.1 vs. 11.2±10.1 years, p < 0.001). Disease activity was lower (DAS-28 3.0±1.2 vs. 4.7±1.3, p<0.001) and functional status was higher (HAQ-DI 0.62±0.37 vs. 1.18±0.82) prior to bDMARD treatment, in ERA patients. Following the onset of symptoms, patients with ERA were monitored for 17 years, whereas those with polyarticular arthritis were monitored for 23 years. At the last follow-up, patients with polyarthritis have higher disease activity, lower functional status, and increased need for prosthesis (Table 1).
Conclusion: Childhood ERA mimics spondyloarthritis in adulthood, whereas polyarticular arthritis resembles rheumatoid arthritis [2]. Indeed, gender and treatment preferences support this differentiation. The duration between the diagnosis of the disease and the beginning of bDMARD was longer in individuals with polyarticular arthritis than in those with ERA. When high disease activity, poor functional status, and, particularly, the frequency of hip prosthesis are considered together, it is possible to predict that polyarticular arthritis will have a worse prognosis after approximately 20 years of follow-up, and it may be more appropriate for these patients to begin intensive treatment earlier.
REFERENCES: [1] Foster HE, Marshall N, Myers A, Dunkley P, Griffiths ID. Outcome in adults with juvenile idiopathic arthritis: a quality of life study. Arthritis Rheum. 2003 Mar;48(3):767-75.
[2] Oliveira-Ramos F, Eusébio M, M Martins F, et al. Juvenile idiopathic arthritis in adulthood: fulfilment of classification criteria for adult rheumatic diseases, long-term outcomes and predictors of inactive disease, functional status and damage. RMD Open. 2016 Sep 22;2(2):e000304.
Table 1. Demographic and Clinical Characteristics of Patients with Enthesitis-Related Arthritis and Polyarticular Arthritis
Acknowledgements: NIL.
Disclosure of Interests: None declared.