

Background: Psoriatic arthritis (PsA) links to heightened cardiovascular risks, with psoriasis independently tied to myocardial infarction and stroke. Concerns persist regarding PsA treatments like infliximab and secukinumab and their impact on cardiovascular events. While IL-17 inhibitors, including secukinumab, effectively manage PsA symptoms, their role in cardiovascular mortality among PsA patients remains unclear. Current limited data suggest IL-17 inhibitors might not substantially impact cardiovascular outcomes. Yet, in-depth studies are imperative to comprehend their influence on cardiovascular mortalities in PsA for precise patient management.
Objectives: In an observational, retrospective cohort study, we explored the correlation between the usage of tumor necrosis factor alpha inhibitors (TNFi) and interleukin 17 inhibitors (IL-17i) in managing PsA. Leveraging the TrinetX database encompassing electronic health records from 75 diverse global healthcare organizations, our objective was to analyze and compare the incidence of cardiovascular events among PsA patients receiving these distinct biologic therapies.
Methods: In this study, our focus was on patients aged 18 and above diagnosed with diagnosis of PsA using International Classification of Diseases, Tenth Revision (ICD-10) codes. Analysis involved the timeline from January 1 st ,2000 through December 14 th , 2023. Two cohorts were created: those receiving treatment with TNFi – Infliximab, adalimumab, certolizumab pegol, golimumab, and etanercept (confirmed via RxNorm codes), and those treated with IL-17i - Brodalumab, ixekizumab, and secukinumab. The analysis excluded individuals undergoing alternative biologic or non-biologic therapies. Index event was defined as the initial appearance of the PsA diagnosis and corresponding medication in the patient records. We utilized propensity score matching for age at the index event, sex, race/ethnicity, and diagnoses of psoriasis or skin diseases. Our outcomes of interest encompassed the incidence of ischemic heart diseases and heart failure. Patients displaying these outcomes before the index event were excluded from analysis. Employing measures of association, we calculated risks and risk ratios to investigate the potential correlation between the utilization of TNFi or IL-17i and the occurrence of ischemic heart diseases and heart failure in patients diagnosed with PsA.
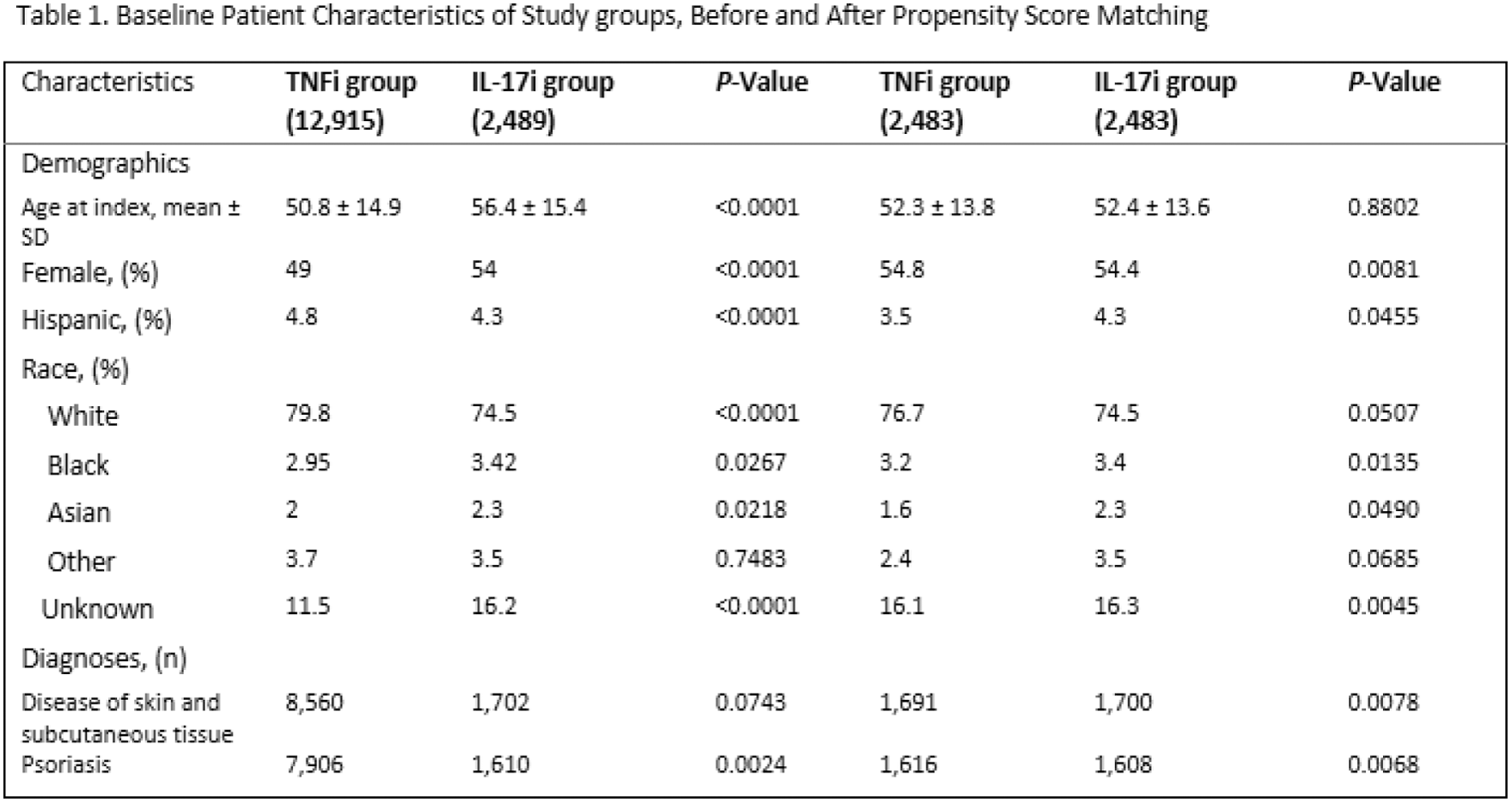
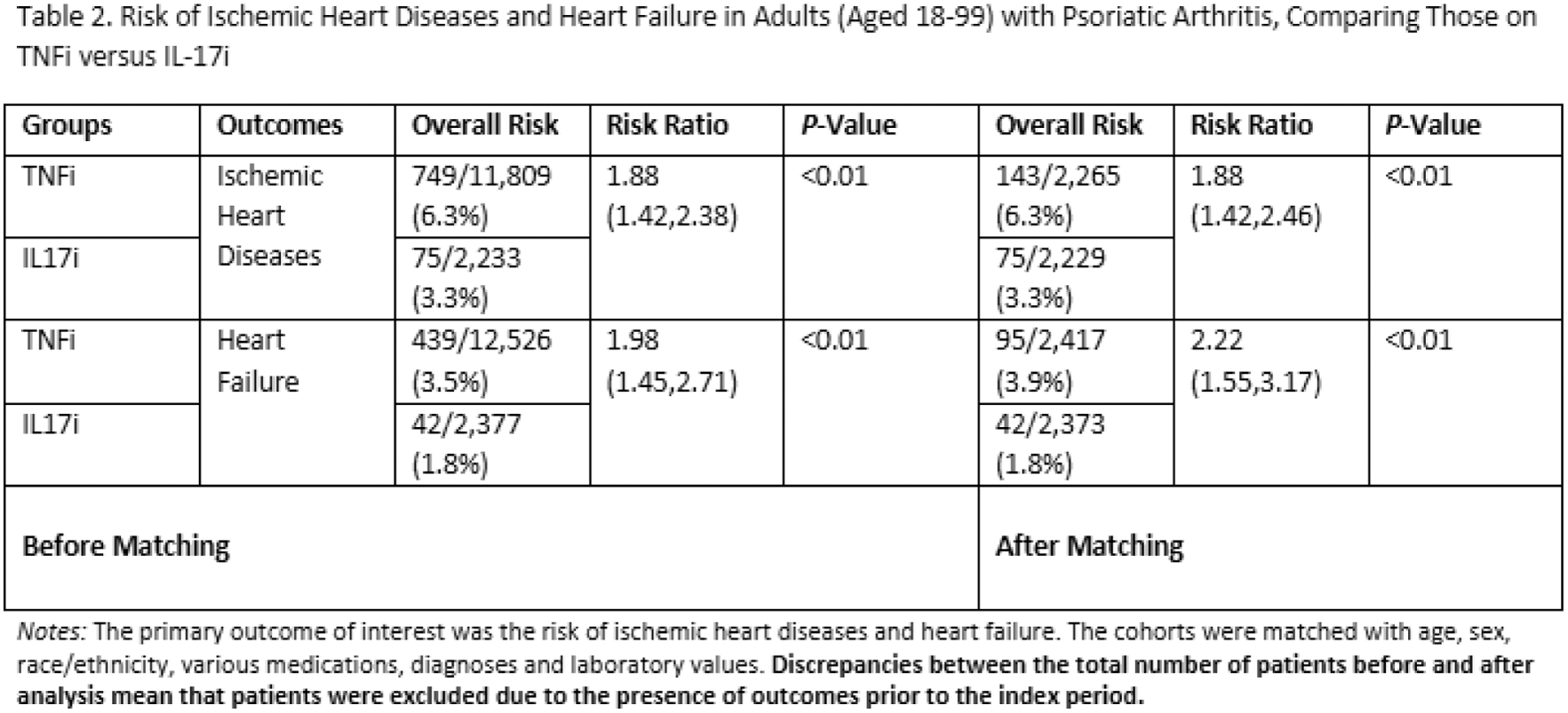
Results: Following the initial analysis involving 12,915 patients receiving TNFi and 2,489 patients receiving IL-17i, slight age differences were noted between the groups before matching. Both groups predominantly comprised over 70% white patients, with a nearly equal distribution of sexes, leaning slightly towards females. Additionally, a majority in both groups had recorded diagnoses of cutaneous psoriasis (Table 1). Before propensity score matching, findings revealed a higher risk of ischemic heart diseases among patients in the TNFi group (6.3%) compared to the IL-17i group (3.3%) with a relative risk (RR) of 1.88 (95% CI 1.42-2.38, p <0.0001). The risk of heart failure was also elevated in the TNFi group (3.5%) in contrast to the IL-17i group (1.8%) with an RR of 1.98 (95% CI 1.45-2.71, p<0.001). After propensity score matching, wherein 2,483 patients from each group were included in the analysis, the results reaffirmed the higher risks observed in the TNFi group for ischemic heart diseases (6.3% vs. 3.3%) with an RR of 1.88 (95% CI 1.42-2.46, p <0.0001). Similarly, the elevated risk of heart failure persisted in the TNFi group (3.9%) compared to the IL-17i group (1.8%) with an RR of 2.22 (95% CI 1.55-3.17, p<0.0001) (Table 2).
Conclusion: Our study underscores a potentially notable association between tumor necrosis factor alpha inhibitor (TNFi) therapy in psoriatic arthritis (PsA) and an increased risk of ischemic heart diseases and heart failure compared to interleukin 17 inhibitor (IL-17i) treatment. These findings emphasize further investigation to comprehensively delineate the underlying mechanisms driving these observed associations and their clinical implications.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.