

Background: Blocking interleukin-6 (IL-6) receptor (IL-6R) with tocilizumab (TCZ) has demonstrated effectiveness in reducing Giant Cell Arteritis (GCA) flares and sparing glucocorticoids (GCs) [1,2] but little is known about the functional role of IL-6 and the impact of TCZ on signalling pathways and cell responses in GCA vascular lesions. The impact of TCZ on imaging abnormalities is confounded by concomitant GC use and there is a concern about whether TCZ really modifies vascular inflammation or provides a valuable symptomatic relief only.
Objectives: The aim of this study was to explore expression and functional roles of IL-6 and IL-6R in GCA and to assess effects of TCZ on GCA vascular lesions.
Methods: 29 GCA temporal artery biopsies (TABs) and 16 normal TABs were included. TAB sections were cultured with or without TCZ (10µg/mL, Roche) or with control IgG (10µg/mL, Sigma). mRNA encoding candidate molecules (n=40) according to the current pathogenesis model, which included transcription factors, cell markers, cytokines, chemokines, adhesion molecules, growth factors, metalloproteases, and matrix proteins, were explored by qRT-PCR and protein was assessed by immunofluorescence or western blot in tissue or ELISA in the supernatants. Adhesion and chemotaxis assays were also performed.
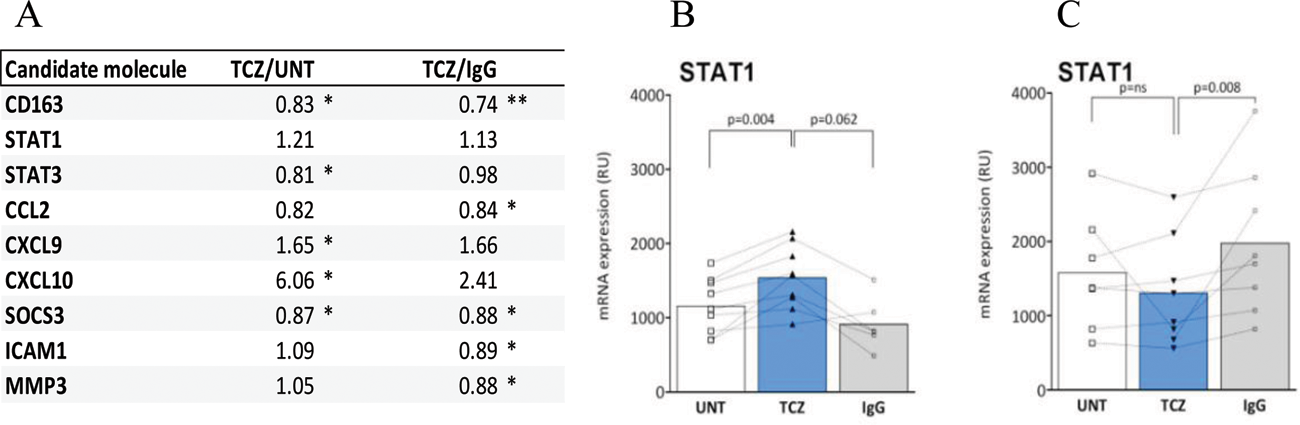
Results: IL-6 and IL-6 R expression by inflammatory cells and resident cells (vascular smooth muscle cells [VSMC] and endothelial cells) is increased in GCA tissue. TCZ treatment decreased expression/phosphorylation of STAT3 and reduced expression of STAT-3-dependent molecules including SOCS3, CCL-2, ICAM-1(Figure 1 A). Accordingly, TCZ reduced adhesion and chemotaxis of PBMC to primary VSMC and endothelial cells (HUVEC). In half of TABs, TCZ decreased and in the other half, increased STAT-1 (Figure 1 B-C) expression/phosphorylation and expression of STAT-1- dependent chemokines including CXCL9 and CXCL10.
mRNA expression (ratio) of most relevant candidate molecules (A) and mRNA expression of STAT1 (B, C) in GCA cultured arteries treated with or without TCZ or non-immune IgG. STAT1 results are separated according to whether IL6 blockade increased (B) or decreased (C) STAT1 mRNA levels.
Conclusion: Our results indicate that TCZ has an impact on relevant inflammatory pathways in GCA tissue, probably resulting in decreased recruitment of inflammatory cells into lesions. Response was not homogeneous and about half of the patients are able to activate alternative inflammatory pathways in their lesions as a potential escape mechanism to TCZ. Funded by AEI (PID2020-114909RB-I00) and the Vasculitis Foundation; FK: ITN-HELICAL (MSCA No.813545).
REFERENCES: [1] Stone JH, et al. NEJM 2017.
[2] Weyand CM, Fulbright J W, Hunder G G, Evans J M, Goronzy J J. Arthritis Rheum. 2000.
Acknowledgements: NIL.
Disclosure of Interests: Roser Alba-Rovira: None declared, Farah Kamberovic: None declared, Marc Corbera-Bellalta: None declared, Ester Planas-Rigol: None declared, Marco A Alba: None declared, Sergio Prieto-González Boehringer, José Hernández-Rodríguez: None declared, Georgina Espígol-Frigolé VIFOR and GSK, VIFOR, GSK and JANSSEN, GSK, Maria C. Cid GSK, AbbVie, CSL-Vifor and Astrazeneca, GSK, AbbVie, CSL-Vifor and Astrazeneca, Kiniksa Pharmaceuticals Corp.