

Background: Behcet’s disease (BD) is a multisystem autoinflammatory disorder characterized by recurrent oral and genital ulcerations, skin lesions, uveitis, as well as vascular, neurological, and gastrointestinal manifestations[2]. Due to the heterogeneity of clinical manifestations, treatments appear to be differentially effective in patients with different systems involved[1]. The pathogenesis of BD is poorly understood and some of the critical questions remain unresolved in BD management including duration and choice of treatments for different subtypes of BD patients and “treat-to-target” strategies, etc.
Objectives: This study aimed to identify immunological signatures among different subtypes of BD patients and look for theoretical basis for further precise targeted therapy.
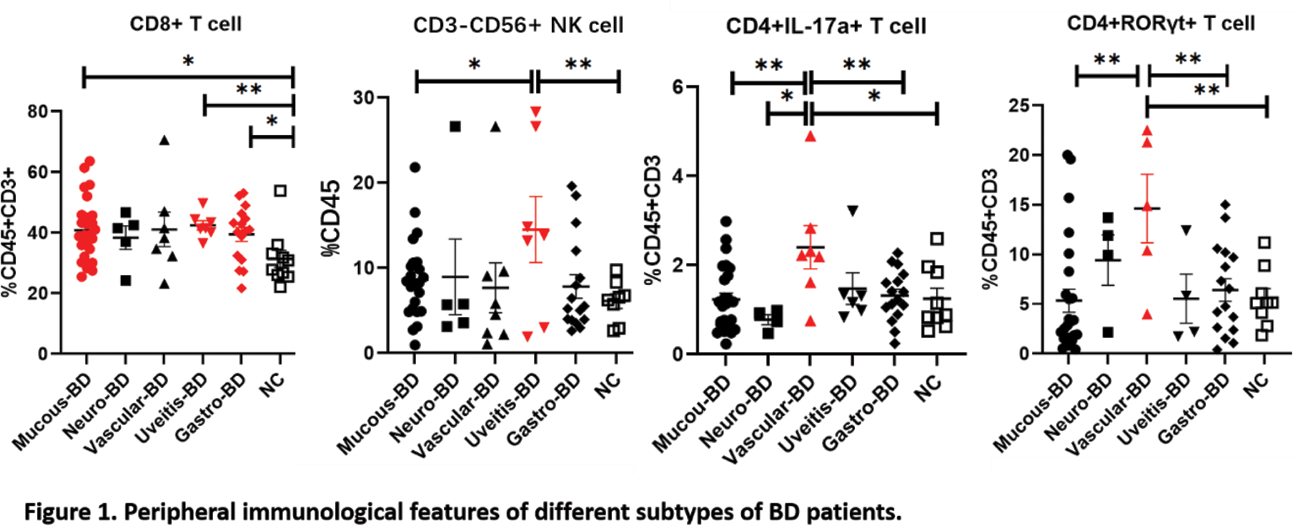
Methods: The landscape of 20 immune-cell phenotypes in the peripheral blood were measured by multi-color flow cytometry from 58 BD patients including 25 mucocutaneous type, 6 uveitis, 4 with central nervous system affected, 7 with vascular manifestation, 16 with gastrointestinal ulceration as well as 9 healthy donors. Statistical differences in quantitative parameters among two groups were determined using unpaired t test. Differences were considered statistically significant at P<0.05.
Results: The population of CD3 + CD8 + T cells in the blood of patients with mucocutaneous type, uveitis and gastrointestinal type were remarkably increased and higher than normal controls (P<0.05). In addition, the peripheral proportion of CD3 - CD56 + NK cells in BD patients with uveitis was higher than that of normal controls, and was also significantly higher than that of mucocutaneous BD patients (P<0.05). Compared with other subtypes of BD patients, the proportion of CD4 + IL-17A + and CD4 + RORγt + T cells in the peripheral blood of patients with vascular manifestation were not only higher than that of normal controls, but also remarkably increased in patients with mucocutaneous type (Figure 1).
Conclusion: Peripheral immunological features may have the potential to stratify BD patients with different organ involved, which may have implications for precise target therapy selection.
REFERENCES: [1] Liu, H., Zhang, P., Li, F., Xiao, X., Zhang, Y., Li, N., Du, L. & Yang, P. (2023) Identification of the immune-related biomarkers in Behcet’s disease by plasma proteomic analysis. Arthritis Res Ther , 25 , 92.
[2] van der Houwen, T.B., van Hagen, P.M. & van Laar, J.A.M. (2022) Immunopathogenesis of Behcet’s disease and treatment modalities. Semin Arthritis Rheum , 52 , 151956.
Acknowledgements: Professor Chen Dong, Westlake University School of Medicine.
Disclosure of Interests: None declared.