

Background: Ultrasound (US) and cranial MRI, with a contrast enhanced, 3T T1-weighted, fat saturated “black blood” sequence (T1fs-BB), are both recommended for suspected giant cell arteritis (GCA). [1] For US, the presence of a halo and/or compression sign has typically been relied on to diagnose GCA, but recently cut-off values for the intima-media thickness (IMT) have also been used. Cardiovascular risk (CVR) is known to influence the IMT.
Objectives: To compare the diagnostic accuracy of cranial 2D T1fs-BB MRI and US of the temporal arteries (TAs) for suspected GCA. To evaluate the influence of CVR on diagnostic accuracy.
Methods: Retrospective, single center study at vasculitis referral center. Inclusion criteria: ≥ 50 years of age; evaluated for suspected GCA between 1.1.2018 and 31.12.2021; available T1fs-BB MRI and US of the TAs. Exclusion criteria: missing informed consent; severe image artifacts; non-GCA vasculitis; interval between modalities > 7 days. Diagnostic reference: clinical expert diagnosis after ≥ 6 months. Patients with atherosclerotic diseases, diabetes mellitus (unless <10 years duration and no end-organ damage/additional risk factors), moderate/severe renal insufficiency or familial hypercholesterolemia, were considered at high to very high CVR according to 2021 European Society of Cardiology guidelines. 3T T1fs-BB sequences were acquired according to EULAR recommendations. [1] Enhancement and wall thickening of bilateral TA segments (common superficial TA, parietal/frontal branches), posterior auricular and occipital arteries were re-rated on a scale from 0 to 3; grades 2 and 3 were considered as vasculitis. [1] Results of US scans, performed with 18 or 22 MHz probes, were retrieved from patient records. The following US protocol is used at the study center: TAs segments are examined bilaterally from below the tragus to the level of the central frontal hair line; halo and/or compression sign are rated and the compressed IMT is measured in transverse view in B-mode and outside of atherosclerotic plaques. US results were assessed in three different variants: US-1 “IMT Cut-Off”: IMT above segmental cut-offs (values by Schäfer et. al. multiplied by two [2]); US-2 “OMERACT”: presence of halo and/or compression sign; US-3 “Expert opinion”: according to rheumatologist who performed the US, as documented on written report.
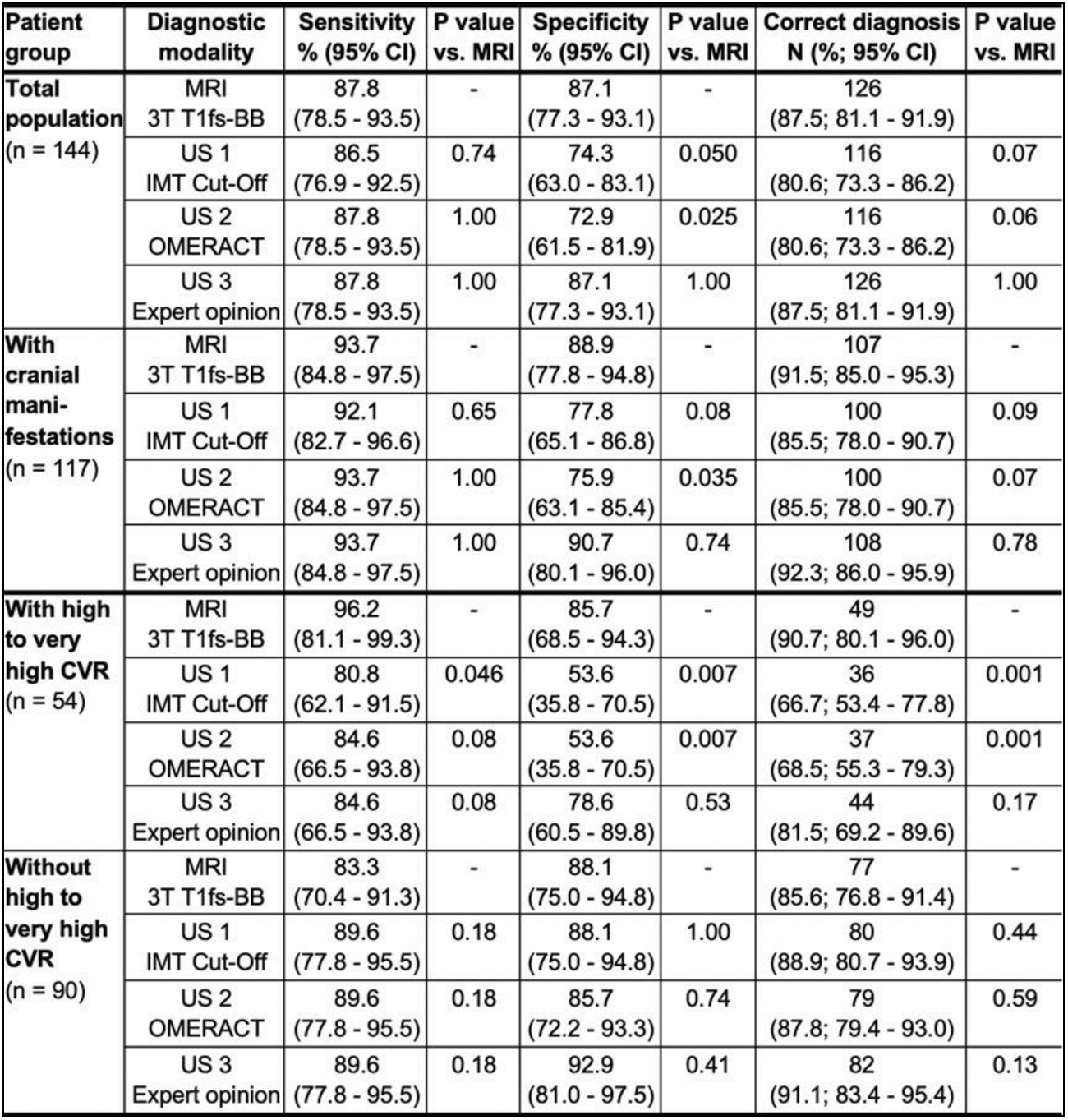
Results: A total of 223 patients met the inclusion criteria, 79 were excluded; the final population consisted of 144 patients (74 (51.4%) with GCA (72/74 fulfilled the 2022-ACR/EULAR criteria) and 70 (48.6%) without GCA). The mean age was 71 years, 59% were female, 54 (37.5%) patients had a high to very high CVR. 79/144 (54.9%) patients had a TA biopsy; 42/55 (76.4%) with GCA had a positive biopsy. Timing of US and MRI: US before MRI in 61 (42.4%), MRI before US in 37 (25.7%), MRI and US on the same day in 46 (31.9%) patients. Glucocorticoids were started before US in 51 (35.4%) patients, median duration of 0 d (interquartile range (IQR) 0-2 d) and before MRI in 48 (33.3%) patients, median duration of 0 d (IQR 0-3 d). Binary agreement between MRI and US was 79.2% to 83.3% for the patient level and 84.7% to 85.0% for the segment level (for TAs). The sensitivity, specificity, and proportion of correct diagnosis of three different US variants compared to T1fs-BB MRI for four patient groups are shown in the Table 1.
Conclusion: For the total population and in patients with cranial manifestations, T1fs-BB MRI outperformed US assessment according to OMERACT or using IMT cut-offs due to its higher specificity. The expert opinion of the physician performing the ultrasound revealed almost identical results, possibly due to the inclusion of CVR into the final assessment. For patients without high to very high CVR, US and MRI perform equally well; for patients with high to very high CVR, MRI shows a better diagnostic accuracy. Different IMT cut-offs seem justified for patients with high to very high CVR.
REFERENCES: [1] Dejaco C, et al. Ann Rheum Dis. 2023-224543. 2) Schäfer VS, et al. Rheumatology 2017. Sep 1;56(9):1479-1483.
Acknowledgements: NIL.
Disclosure of Interests: Luca Seitz: None declared, Susana Bucher: None declared, Britta Maurer Boehringer-Ingelheim, GSK, Novartis, Otsuka, MSD, Novartis, Boehringer Ingelheim, Jannsen-Cilag, GSK, Novartis, Franca Wagner Not related to the topic, Research support, not related to the topic, Fabian Lötscher: None declared, Pascal Seitz: None declared.