

Background: The theoretical gain of value-based healthcare (VBHC) is widely embraced: VBHC improves patient-relevant outcomes in relation to patient journey costs. However, evidence on the impact of transforming care organizations into a well-functioning integrated VBHC unit is missing. So far, care organizations have not completed all reinforcing steps towards VBHC. Patient-centered care (PCC) has not been put at the heart of VBHC, due to limited focus on outcomes that matter to patients. Moreover, the denominator of VBHC, costs, has not been incorporated, leaving the equation of VBHC on outcomes and costs unevaluated. Therefore, over the past years an (digital) integrated practice unit (IPU) was established named “ Joint Value ” that aims to continuously create and deliver better, and more value for all healthcare stakeholders.
Objectives: We provide a practical roadmap on how to implement VBHC, including PCC, as a well-working IPU. This can be used as an inspiration and guidance to other hospitals and providers in primary care.
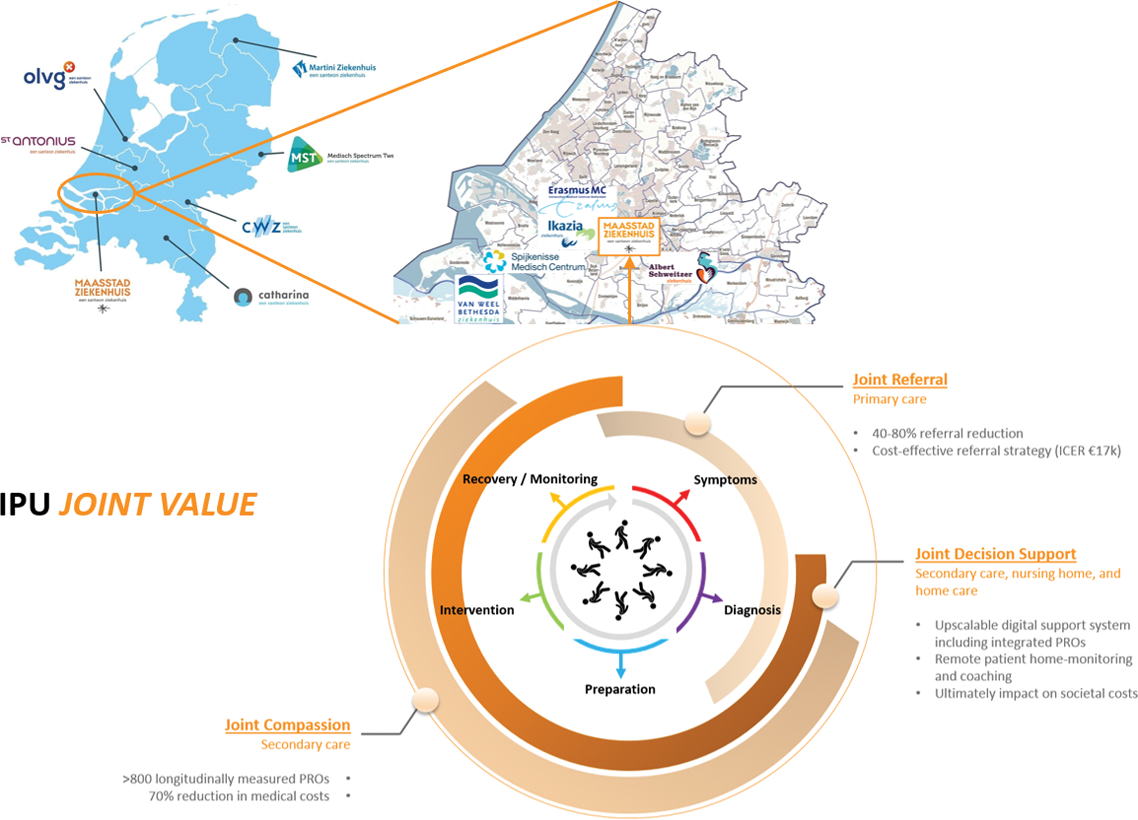
Methods: As a case study, we use the transformation of the rheumatology department at the Maasstad Hospital, the Netherlands where three main programs were initiated to gradually move towards an IPU. These are practical examples on how to fulfill the six steps model based on Porter and Lee and the Value Agenda for the Netherlands. Moreover, a patient partner panel was employed to identify urgent care-cycle improvements that we initiated between 2014 and now, including: optimizing referrals to the rheumatology departments, outcome data-visualization on the individual and group level, and support in self-management over time.
Results: Next to providing a practical roadmap, we show that VBHC in combination with PCC induces improvements in healthcare on the individual patient (micro), rheumatology department (meso) and regional and national providers (macro) level. On the micro level, we established a patient-reported outcome integrated dashboard for shared decision-making, telemonitoring and coaching. On the meso level, we worked on improving the patient journey, which led to a reduction of 40-80% in the number of referrals from primary to secondary care. Also, we learn from health technology assessment on how to operationalize the value equation. On the macro level, we are the first to collect real-world data on clinical and patient-reported outcomes between rheumatology departments and hospitals to learn from each other. The Santeon benchmark led to 70% cost reduction for biologicals.
Conclusion: We have established a roadmap that can be adapted to multiple indications and healthcare divisions with the potential to serve as an evidence-based VBHC blueprint. However, more evidence is needed on how to operationalize the value equation, and which methods can be used to measure this, which is part of our research for 2024.
REFERENCES: NIL.
Overview and impact of IPU “Joint Value” .
Acknowledgements: On behalf of the JOINT VALUE network. Cooperation partners: Erasmus School of Health Policy & Management, Learnpoint Koel, Macaw, Microsoft, National Society Reumazorg Nederland, and Dutch National Health Care Institute.
Disclosure of Interests: None declared.