

Background: Rheumatoid arthritis (RA) is a chronic, autoimmune, and inflammatory disease. Cardiovascular (CV) disease in the main cause of death in this population due to the presence of proinflammatory cytokines, contributing to the development of atherosclerosis and endothelial damage. CV risk algorithms for the general population have shown to underestimate the real CV risk in RA patients. The American Heart Association published the Predicting Risk of CV disease EVENTs (PREVENT TM ) algorithm in 2023 to assess the risk of developing atherosclerotic CV disease in 10 years [1].
Objectives: We aimed to assess the concordance of high-risk classification according to the 2023 PREVENT TM algorithm and to the presence of carotid plaque (CP) in RA patients, and to determine the proportion of patients reclassified to high CV risk with the carotid ultrasound.
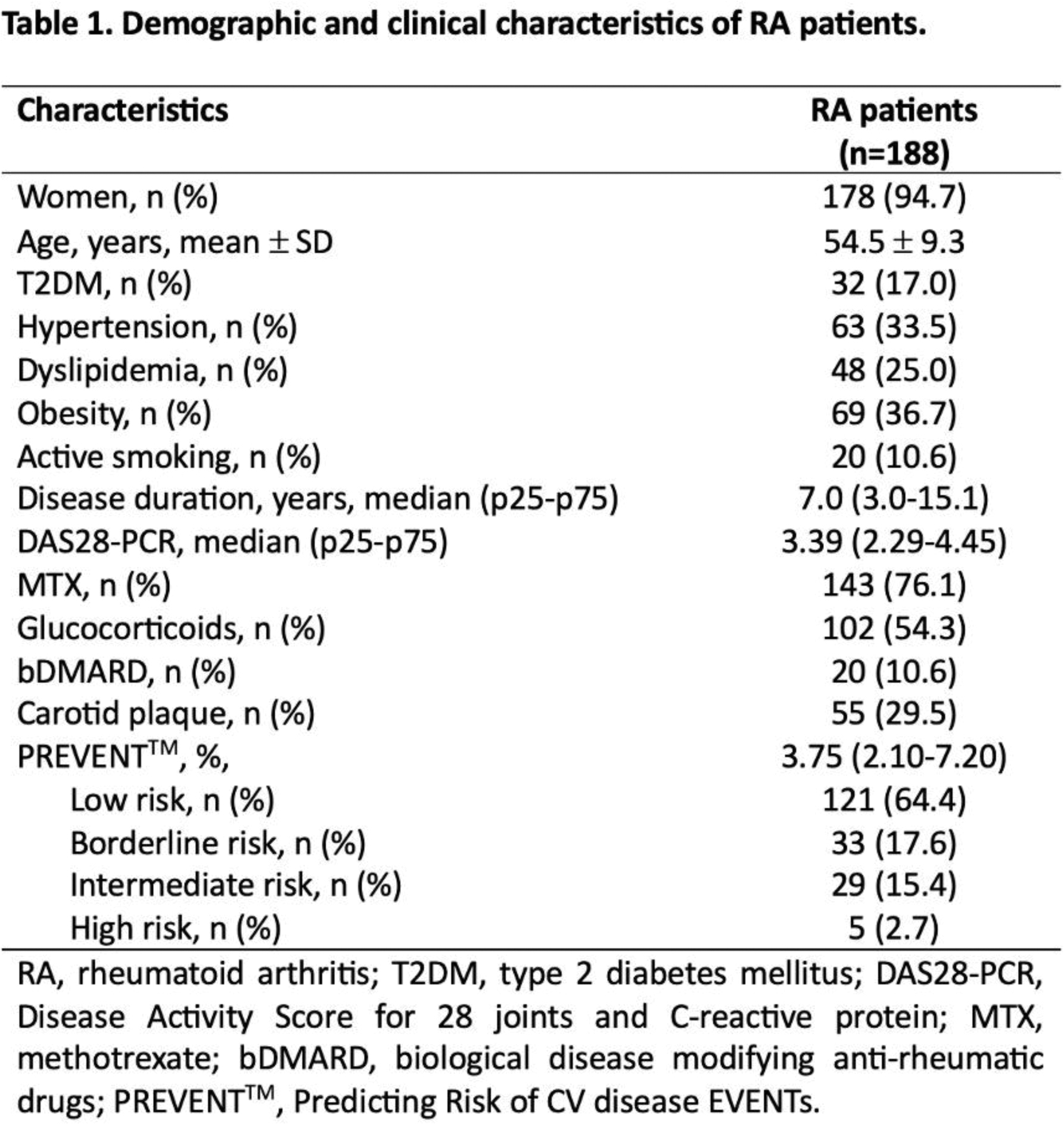
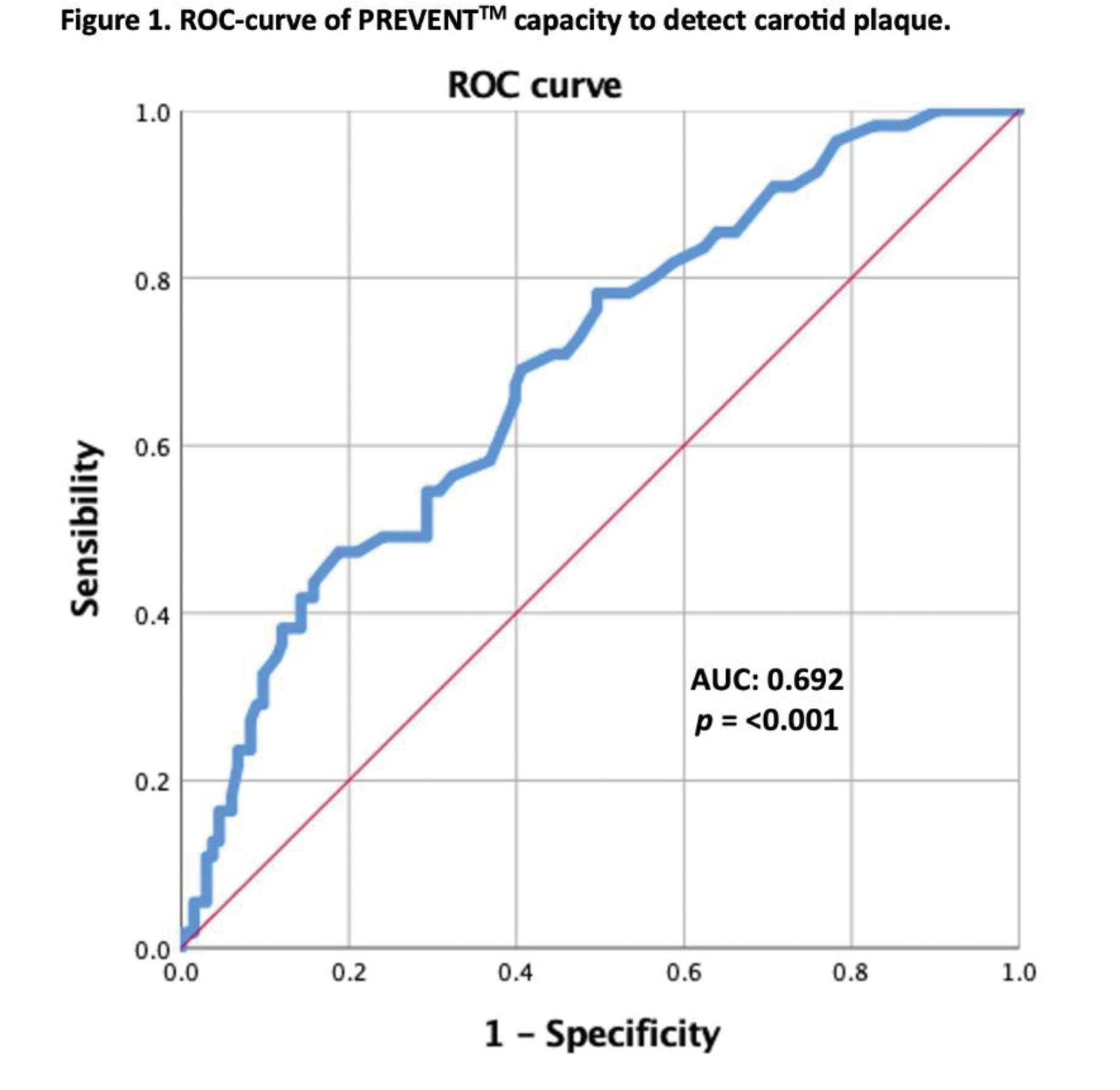
Methods: Cross sectional study. We recruited 188 RA patients who fulfilled the 2010 ACR/EULAR classification criteria, aged 30-79 years. Patients with a previous CV event, overlap syndrome, pregnancy or current/previous treatment with statins were excluded. CV risk was assessed with the PREVENTTM algorithm. The results were multiplied by 1.5, according to current guidelines. A carotid ultrasound was performed to all patients, and the presence of CP was considered as a carotid intima media thickness ≥ 1.2 mm, or a focal narrowing ≥ 0.5 mm. High risk was defined as the presence of CP or a PREVENTTM algorithm score ≥ 20%. Cohen’s kappa (k) coefficient was used to evaluate the concordance of high-risk classification. A ROC-curve analysis was performed to evaluate the capacity of the PREVENTTM algorithm to identify patients with CP. The cutoff point was determined with the Youden Index.
Results: Demographic and clinical characteristics in Table 1. The PREVENTTM algorithm classified 5 (2.7%) patients in the high-risk category. CP was identified in 55 (29.3%) patients, classifying these patients as high risk. CV risk reclassification by the presence of CP was observed in 52 (27.7%) patients. Of the reclassified patients, 26 (50%) belonged to the low-risk category, 10 (19.6%) belonged to the borderline-risk category and 16 (30.8%) belonged to the intermediate-risk category. There was no concordance between the PREVENTTM algorithm and the carotid ultrasound for high CV risk classification (k = 0.054). The ROC-curve analysis showed an AUC 0.692 (95% CI 0.611-0.773, p = <0.001), sensibility of 67.3% and specificity of 60.2%, with a cutoff point of 3.9% (Figure 1).
Conclusion: This study showed that the PREVENT TM algorithm failed to identify a large proportion of patients classified as high CV risk by the carotid ultrasound and that there was no concordance between both methods. Furthermore, most reclassified patients initially belonged to the low-risk category. The cutoff point to identify patients with CP was 3.9%, which classifies patients as low risk. This algorithm did not show a good performance in identifying high-risk patients; therefore, a carotid ultrasound should be considered as part of the CV risk assessment in RA patients.
REFERENCES: [1] Khan SS, Matsushita K, Sang Y, Ballew SH, Grams ME, Surapaneni A, et al. Development and Validation of the American Heart Association Predicting Risk of Cardiovascular Disease EVENTs (PREVENT) Equations. Circulation. 2023 Nov 10.
Acknowledgements: NIL.
Disclosure of Interests: None declared.