

Background: Up to 20% of lupus nephritis diagnosed within 1 year of lupus diagnosis ends up in end-stage kidney disease (ESKD). Increasing evidence suggests that findings from a second biopsy provide more information regarding the risk of lupus nephritis flare, treatment response, and the development of ESKD.
Objectives: Our study aimed to investigate the predictive value of clinical, laboratory, and histological parameters upon repeat renal biopsy in relation to the development of chronic kidney disease (CKD). Additionally, we assessed the impact of these findings on the treatment of lupus nephritis (LN).
Methods: Patients diagnosed with biopsy-proven LN, fulfilling the SLICC criteria during 2008-2018, were included in this study, and patients were followed up until July 2023. LN classes were divided into proliferative (class III, IV, III+V, IV+V) and non-proliferative (class II, V), and class switch in repeat biopsies was analysed. Clinical and laboratory data at the 1st visit and follow-up visit until July 2023 were recorded. Histopathological findings and simultaneous clinical data at the first and second biopsy were recorded and analysed for clinically significant class changes defined by changes from non-proliferative to proliferative LN and vice versa. Multivariable Cox regression models were created to predict CKD-free survival. CKD was defined as an eGFR of <60 ml/min/1.73 m2 on at least two occasions, 90 days apart.
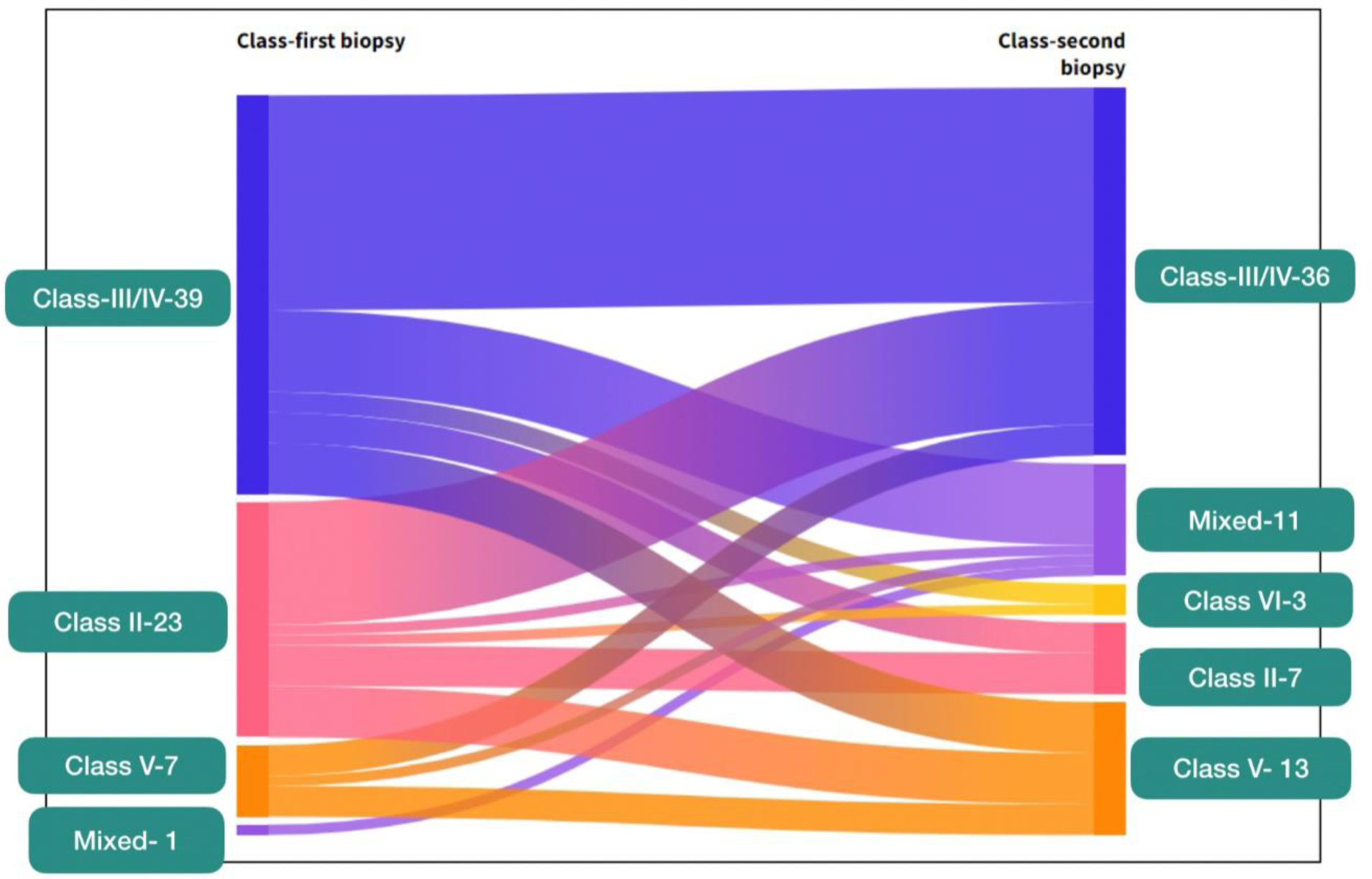
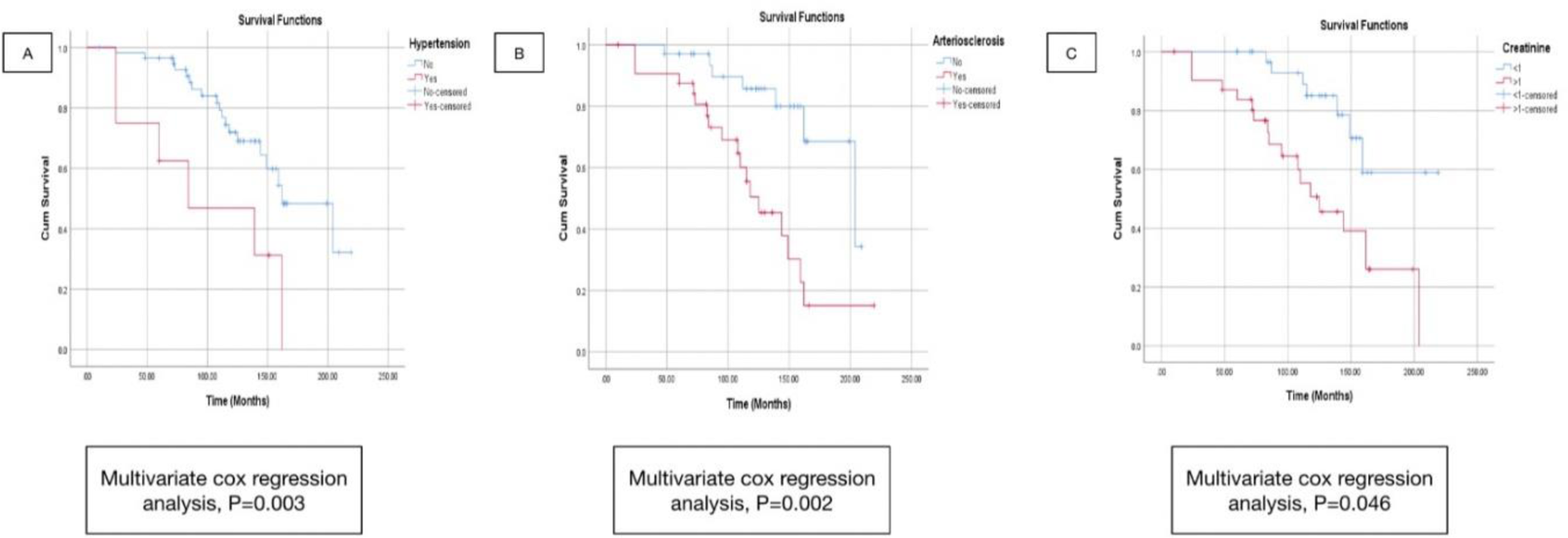
Results: Among the 1100 patients diagnosed with biopsy-proven LN, 90 underwent a second renal biopsy. Seventy patients [65 (93%) women; mean follow-up: 112±46 months] with at least two renal biopsies were identified after exclusion. The indications for re-biopsies included LN flare [n=42, including nephrotic flare (n=13), nephritic flare (n=12), nephritic-nephrotic flare (n=11), elevated creatinine (n=6)] and persistent sub-nephrotic proteinuria (n=28). ISN-RPN histological clinically significant class switches in the second biopsy when compared to the 1st were observed in 35.7% (Figure 1). None of the clinical variables at baseline and follow-up visits in regression predicted the class switch. A total of 25 patients developed CKD after a mean follow-up of 112±46 months. The presence of hypertension at the first renal biopsy (HR 95% CI 5.27 (1.79-15.6), p=0.003), creatinine > 1 mg/dL at the second biopsy (2.85(1.02-7.96), p=0.046), and arteriosclerosis in the second biopsy (5.32(1.86-15.2), p=0.002) were identified as independent clinical and histological predictors of CKD-free survival (Figure 2). No histological parameter at the first biopsy predicted CKD-free survival. Nineteen (27.1%) patients who were considered to have clinical renal activity in the form of active urinary sediments and elevated creatinine had the presence of only chronic changes or switched to lower classes in repeat biopsy, leading the clinician to not escalate or de-escalate the immunosuppression.
Conclusion: The presence of arteriosclerosis in the second renal biopsy and concomitant elevated creatinine values predicted the development of CKD in patients with lupus nephritis. A clinically significant class switch affecting treatment decisions was observed in a third of the LN patients following re-biopsy.
ISN/RPS classification at the first and second biopsies using a Sankey diagram
Survival outcomes (CKD free survival) based on Multivariate Cox regression (A) Patients with hypertension at baseline (B) Arteriosclerosis at second biopsy (C) Patients with creatinine >1 mg/dL at second biopsy.
REFERENCES: NIL.
Acknowledgements: Department of nephrology, Department of general pathology, Christian Medical College, Vellore, India.
Disclosure of Interests: None declared.