

Background: The Janus kinase (JAK)-transducer and activator of transcription signal (STAT) pathway is a signaling cascade involved in regulating various cellular processes, including immune responses, cell growth, and differentiation. Several evidence have shown the clinical relevance of interfering with the JAK/STAT activation in modulating clinical manifestations of different inflammatory conditions, including idiopathic inflammatory myopathies (IIM) in the last few years, especially in dermatomyositis (DM) [1]. On the other hand, the role of interferon (IFN) in IIM pathogenesis has been highlighted, with different signatures relating to specific clinical phenotypes. Type 1 IFN signaling is mediated by a heterodimeric receptor, composed of IFNA-R1 and -R2, capable of eliciting the activation of tyrosine kinase-2 (TYK2) and JAK-1, respectively, however, it has not been ascertained which is more important in modulating the subsequent phosphorylation step of the STAT.
Objectives: This study aimed to investigate the activation of the STAT3 protein and the role of the individual subunits JAK-1, -2, -3 and TYK-2 on its phosphorylation in DM patients.
Methods: Blood samples from n.5 DM patients, fulfilling the 2017 EULAR/ACR criteria for IIM [2], and n. 5 healthy blood donors (HD) were collected. DM patients had active disease, 3 were positive for anti-MI2 antibodies, one for anti-TIF1γ antibodies, and one for anti-Ro52 antibodies; all were naïve to corticosteroids and any immunosuppressive drug. Separated peripheral blood mononuclear cells (PMBC) were evaluated for phosphorylated STAT3 levels by fluorescence-activated cell sorting (FACS) analysis, both in CD4 pos and CD14 pos cells, before and after incubation in separated cultures with half-maximal inhibitory concentration (IC50) of abrocitinib, gandotinib, peficitinib, or deucravacitinib (Biovision Inc. – CA, USA), as direct inhibitors of JAK-1, -2, -3 and TYK2, respectively. The cell analysis was performed by Kaluza software (v 2.1, Beckman Coulter) and the GraphPad Instat (v.9.5.1) was used for statistical analysis with appropriate tests.
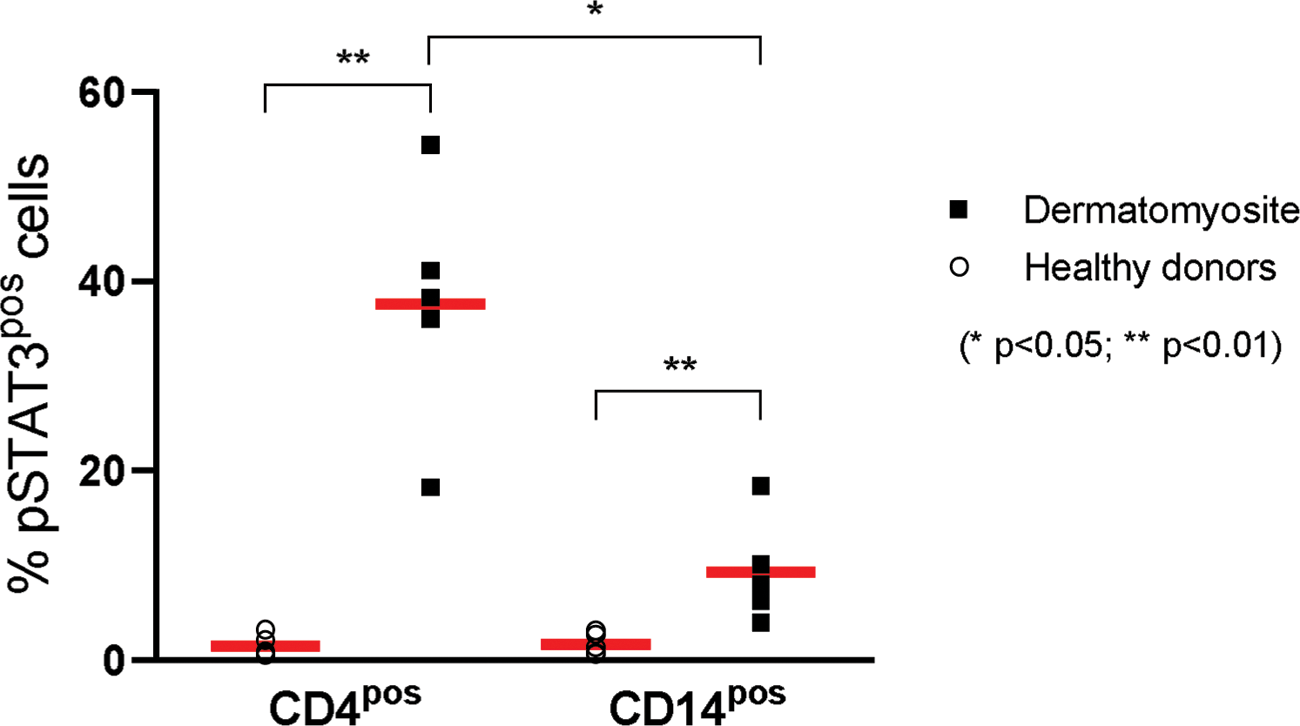
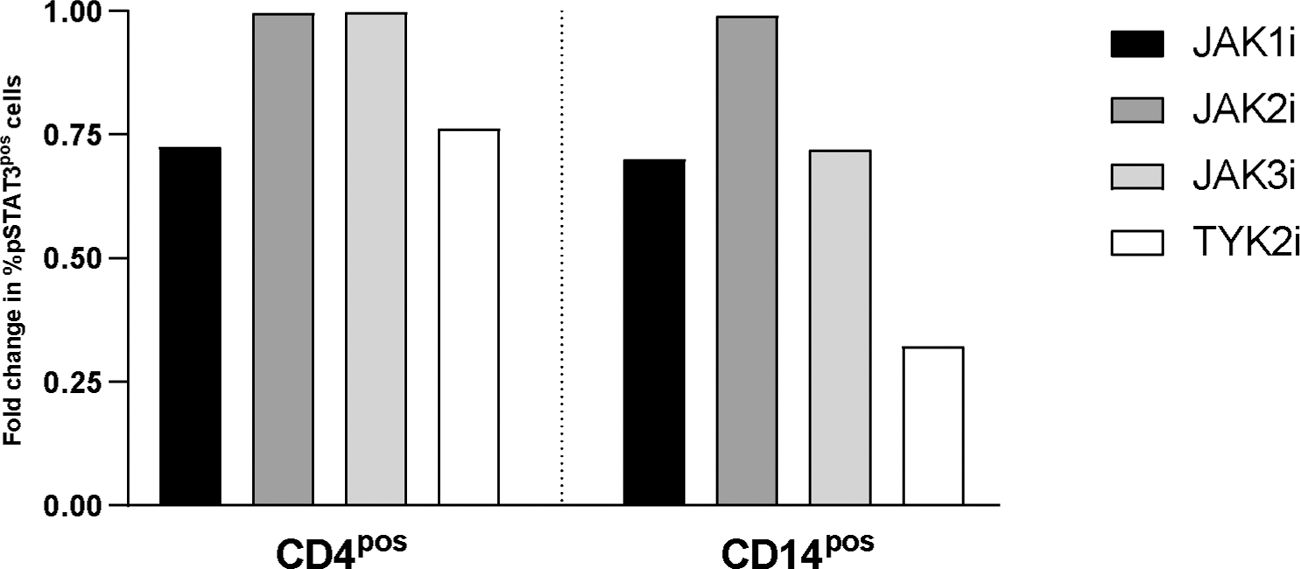
Results: We detected significantly elevated pSTAT3 pos cells in PBMC from IIM compared to HD (p=0.01). In HD we counted a median (95%CI) of 0.9 (0.5-3.2) % CD4 pos - pSTAT3 pos cells and 1.4 (0.7-3.1) % CD14 pos -pSTAT3 pos cells (p=0.73). On the contrary in PBMC from DM we observed a median (95%CI) of 39.7 (18.2-54.4) % CD4 pos - pSTAT3 pos cells and 8.2 (3.9-18.4) % CD14 pos -pSTAT3 pos cells (p=0.01) [Figure 1]. In DM patients the JAK-1 and TYK-2 direct inhibition interfered with the STAT3 phosphorylation of CD4 pos - pSTAT3 pos cells, demonstrating a mean reduction of 28.7% after JAK-1 inhibition and 26.6% after TYK-2 inhibition, compared to un-inhibited cultures. While in CD14 pos -pSTAT3 pos cells after direct JAK-inhibition we observed a reduction of pSTAT3 pos cells of 67.8%, 30% and 28.1% after TYK-2, JAK-1 and JAK-3, respectively. No relevant effect of JAK-2 direct inhibition was observed [Figure 2].
Conclusion: The JAK/STAT3 pathway is significantly activated in patients affected by DM. Specifically, DM patients presented a high activation of pSTAT3 that was modified mainly by direct inhibition of JAK-1 and especially TYK-2 in both lymphocytes and monocytes, thus modulating IFN-I effects. Our findings, to be confirmed in larger studies also evaluating phosphorylation of other STATs, pave the way for the clinical use of JAK-inhibitors in DM patients [3], in particular acting on JAK-1/TYK-2 such as the new brepocitinib.
REFERENCES: [1] Paudyal A, et al. Dermatol Ther. 2021;34(3):e14939.
[2] Lundberg IE, et al. Ann Rheum Dis. 2017;76(12):1955-1964.
[3] Zhang J, et al. Arthritis Res Ther. 2023 Oct 18;25(1):204.
Percentage of pSTAT3 pos in CD4 pos and CD14 pos cells of studied subjects.
Fold change in pSTAT3 pos cells of dermatomyositis patients after culture with direct JAK inhibitors.
Acknowledgements: NIL.
Disclosure of Interests: None declared.