

Background: An incereased frequency of venous thromboembolism (VTE) in ANCA- associated vasculitis (AAV) has been reported previously [1,2]. However it is not clear yet which AAV patient would benefit prophylactic anticoagulant treatment.
Objectives: The aim of the present study is to evaluate the occurence and the associated factors with VTE in a multicenter large national AAV cohort of TR-VAS.
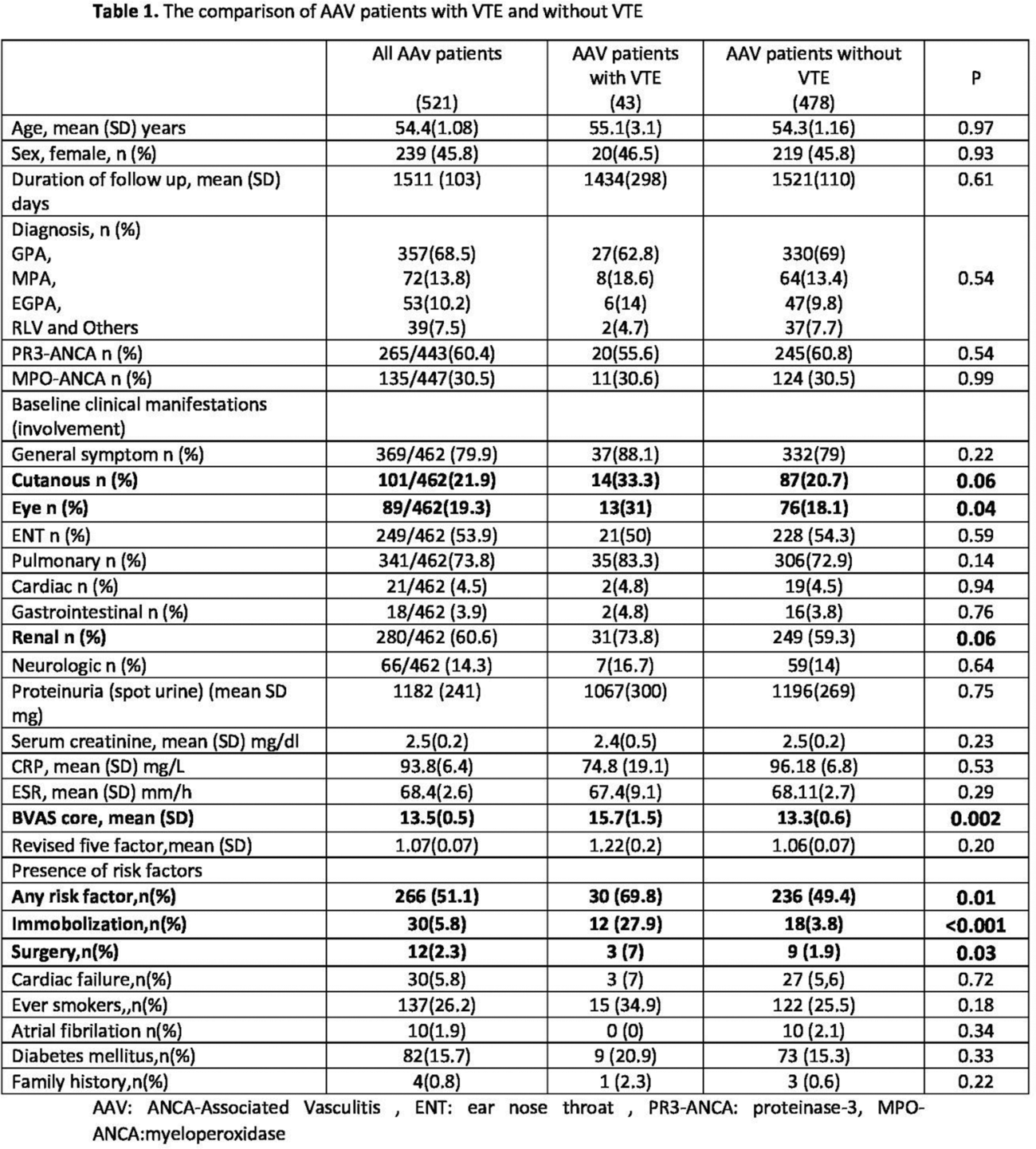
Methods: In this nationwide study, we included patients with granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and unclassified AAV (uAAV) according to the European Medicines Agency algorithm from TRVaS, multicenter, and e-database of Turkey. Data recorded in the TRVaS database (baseline demographic, disease related characteristics [including organ/system involvements, data regarding disease activity and severity], comorbidities, serologic and other laboratory data as well as the treatment initiated for AAV, the development of end-stage renal disease and the survival status during follow up were withdrawn. Additionally, data about VTE were collected from participating centers by using a structured questionnaire. A venous thromboembolic events that occurred within the three months prior the diagnosis of AAV and during the follow up was included in the current analysis. Presence of classical risk factors for VTE (immobilization, trauma, major surgery, malignancy, pregnancy, oral contraceptive use, hormone replacement therapy, heart failure, presence of hematologic disease that may cause thrombosis, smoking history, presence of atrial fibrillation, diagnosis of diabetes mellitus and family history of VTE), disease activity at the time of VTE (BVAS score), antiaggregant/anticoagulant usage were also recorded. The analysis was performed by using the statistical package program [Statistical Package for the Social Science; SPSS 16.0]. A p value of <0.05 was considered statistically significant.
Results: In total, 521 (239 female [45.8], mean age 54.4±1.08 years) patients with AAV were included in the analysis. The majority of the patients was diagnosed as GPA (357/521 [68.5%]) and as expected 60.4% (265/443) of them were PR3-ANCA positive. The demographic and main clinical characteristics of the patients with AAV was summarized in Table 1. In total 43 (8.3%) patients suffered from VTE. When we compared AAV patients with and without VTE (Table 1) we showed that cutaneous and eye involvement was statistically significantly higher (P<0.05) in patients with VTE. Baseline BVAS score was significantly higher in patients with VTE (15.7 ±1.5 vs 13.3 ±0.6 and P=0.002). Although we saw that renal involvement was tended to be higher in patients with VTE this was not reached statistically significance. AAV patients with VTE had higher baseline risk factors for the development of VTE. In multivariate analysis we revealed that baseline BVAS score was the only independent risk factor (OR=1.059, 95% CI 1.008-1.113) for the development of VTE in our AAV patients.
Conclusion: The results of the present study showed that beside well-known risk factors AAV patients with high baseline disease activity, patients in particular with the cutaneous, eye and renal involvement could have higher risk for the devlopment of VTE. The determination of AAV patients with increased risk of VTE would be important to timely start anticoagulant treatment.
REFERENCES: [1] Liapi M, Jayne D, Merkel P, Segelmark M and Mohammad JA. Venous tromboembolism in ANCA-associated vasculitis: a population-based cohort study. Rheumatology 2021; 00:1-8.
[2] Moiseev, Sergey, et al. “Association of venous thromboembolic events with skin, pulmonary and kidney involvement in ANCA-associated vasculitis: a multinational study.” Rheumatology 60.10 (2021): 4654-4661.
Acknowledgements: NIL.
Disclosure of Interests: None declared.