

Background: Axial spondyloarthritis (axSpA) is marked by active sacroiliitis evident through bone marrow oedema (BME) on magnetic resonance imaging (MRI). Traditionally, MRI stands as a cornerstone in axSpA diagnosis. Radiomics emerged as a new frontier in the Rheumatology landscape [1]. Its roots are in oncology, where it has primarily demonstrated its importance in diagnostic and therapeutic prediction. Radiomics involves extracting and analyzing many quantitative features from medical images, including shape, intensity, texture, and spatial relationships, converting imaging into high-dimensional data for further analysis [1].
Objectives: We aimed to explore the associations of the radiomic features of manually segmented BME in sacroiliac joints MRI of axSpA patients with the persistence of TNF inhibitors (TNFi)
Methods: Our analysis included patients with classified axSpA followed at a single centre who underwent MRI scans with a magnetic field > 1 Tesla between January 1
st
2018 and December 31
th
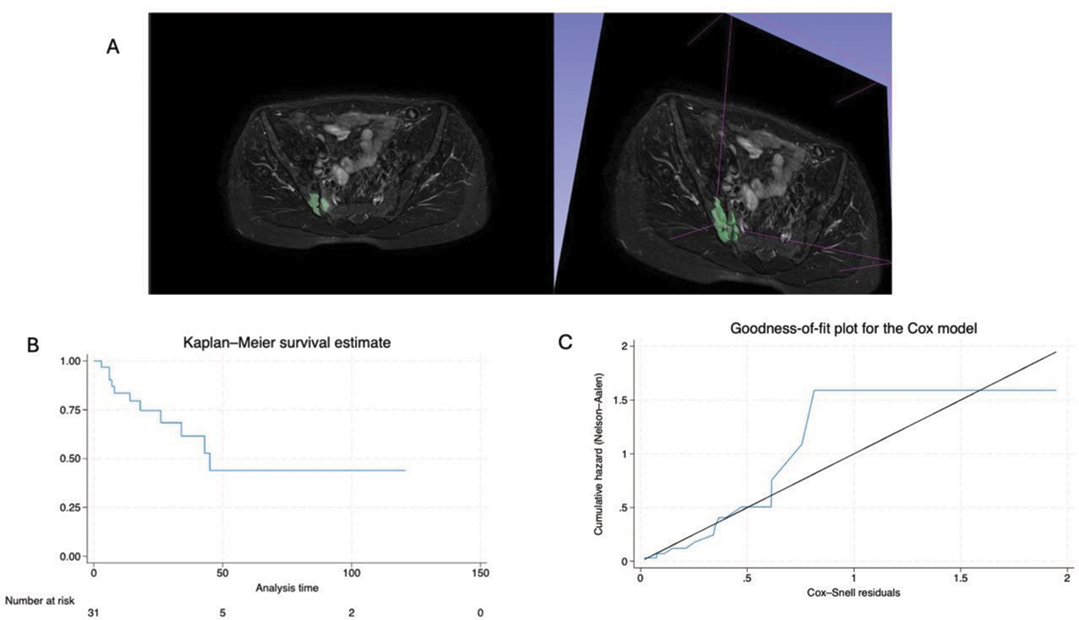
2022. In order to be enrolled such patients had to exhibit active sacroiliitis, as defined by the Assessment of SpondyloArthritis International Society (ASAS) [2]. Due to active sacroiliitis, all the patients started TNFi therapy consequently at the same centre. BME was manually segmented by an expert radiologist on axial scans in a short tau inversion recovery (STIR) sequence using 3D Slicer ver 5.2.1 (Figure 1 Panel A and sample video:
Results: SIJ MRI of 32 patients were included, male 13/32 were (40.6%) with median age (IQR) of 34.5 years (26.50-46.75). Of note, 9 (28.1%) of these 32 patients also fulfilled CASPAR criteria for Psoriatic Arthritis (PsA). Sample features are summarized in Table 1 whereas the mean survival time of the TNFi therapy started after the MRI was 29.22 ±30.35 months (Figure 1 panel B). After checking for autocorrelation, only 39 features were retained. Seven radiomic features showed a significant association with treatment discontinuation at univariate analysis. Therefore, using backward elimination, the model included as radiomic predictors the following features:
Original_shape_Sphericity (HR 2.10, 95%CI 1.09-4.05).
Original_shape_Elongation (HR 0.50, 95%CI 0.25-0.99).
Both predictors reflect BME extension. Cox-Snell VS Nelson-Aalen plot demonstrated that the hazard function followed the 45-degree line very closely except for huge values of time (Figure 1 Panel C).
Conclusion: This proof-of-concept study underscores the potential of radiomic features alone to predict TNF therapy outcomes in axSpA patients. We identified two radiomic features as predictors of anti-TNF survival related to BME extent in SIJ. Such results confirm that BME extension is associated with response to TNFi therapy. Further research is necessary to determine potential confounders; such results ideally need external validation on an independent prospective cohort.
REFERENCES: [1] Venerito V et al. Front Med (2023). 9:1069486.
[2] Lambert RG et al. Ann Rheum Dis. 2016 Nov;75(11):1958-1963.
| Patient Characteristics | Available Obs | |
|---|---|---|
| Male, n (%) | 32 | 13 (40.6) |
| Age at MRI, median (IQR) | 32 | 34.5 (27.50-46.75) |
| BMI, median (IQR) | 32 | 23.63 (21.43-29.78) |
| Disease duration, month, median (IQR) | 32 | 36.0 (12.00-90.50) |
| 1 st line TNFi, n(%) | 32 | 28 (87.50) |
| 2 nd line TNFI, n(%) | 32 | 4 (12.50) |
| ASDAS-CRP at MRI, median (IQR) | 32 | 2.68 (0.26-1.21) |
| HAQ at MRI, median (IQR) | 32 | 0.81 (0.25-1.44) |
Acknowledgements: NIL.
Disclosure of Interests: None declared.