

Background: The diagnosis of primary Sjögren’s syndrome (pSS) is established at a time when symptoms are already present due to tissue damage that has already occurred. Thus, most of our knowledge about the disease is based on a presumed late stage of the autoimmune process that is probably initiated years before the onset of symptoms [1]. This assumption is supported by the lymphopenia often seen in pSS, resulting from a reduced naive T cell compartment. A finding that is likely to be the result of prolonged, continuous immune activation [2].
Objectives: To investigate the clinical, immunological and histological characteristics of individuals at risk of developing pSS.
Methods: This ongoing, longitudinal study included 41 individuals who did not fulfil the ACR/EULAR classification criteria but were considered at risk of developing pSS (defined as anti-Ro antibody positive, OR autoantibody positive first-degree relatives of pSS patients OR patients meeting more than one point of the ACR/EULAR classification criteria). Participants underwent annual study visits for patient- reported outcome measures, pSS- specific clinical assessments and ultrasonography. In addition, laboratory assessments including immune phenotyping of peripheral blood by flow cytometry (FACS) were performed. The FACS measurements were compared with age- and gender-matched healthy controls (HC). Some subjects also underwent salivary gland biopsy followed by an immunohistological staining procedure. The primary endpoint of the study is the diagnosis of pSS or another systemic autoimmune disease (AID).
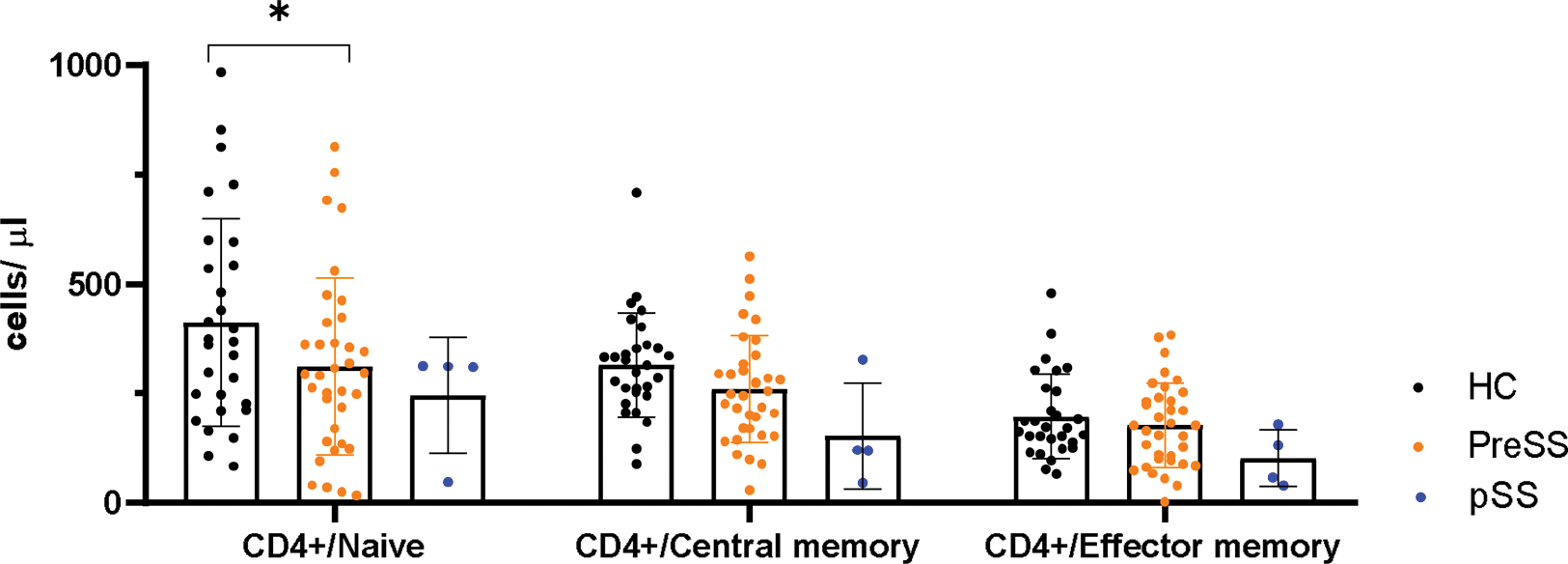
Results: Results from 41 at- risk individuals (female ratio: 0.85; mean ± standard deviation, age: 51 ± 13.27) showed that sicca symptoms were reported by nearly three quarters of participants at baseline (median ± interquartile range, ESSPRI dryness domain: 2 ± 5). 4 individuals already reached the primary endpoint by being diagnosed with pSS (n=3) or rheumatoid arthritis (n=1), respectively. At baseline, only one individual showed pSS- specific changes in the salivary gland ultrasound defined by a Hocevar score above 17 points. When compared to HC, the FACS analysis showed a significant decrease of the CD4+ T cell pool, mostly affecting the naive compartment. This decrease was less profound than in patients with established pSS. The histological analysis already revealed typical features of pSS in some of the individuals at risk (pre- lymphoepithelial lesions in 2/7, defined by presence of intraepithelial B- lymphocytes; plasma cell shift in 3/7, defined by equal amounts of IgG- and IgA- expressing plasma cells).
Conclusion: In this study, we show that individuals at risk of developing pSS already have clinical, immunological and histological features of the disease. The reduction of the naive CD4+ T cell compartment and subtle inflammation of the salivary glands may be a sign of a subclinical disease process that begins before the full clinical picture of pSS is established.
REFERENCES: [1] Olsen NJ, Okuda DT, Holers VM, Karp DR. Editorial: Understanding the concept of pre-clinical autoimmunity. Frontiers in immunology. 2022;13:983310.
[2] Fessler J, Fasching P, Raicht A, Hammerl S, Weber J, Lackner A, et al. Lymphopenia in primary Sjögren’s syndrome is associated with premature aging of naïve CD4+ T cells. Rheumatology (Oxford). 2021;60(2):588-97.
Significant reduction of naive CD4+ T cells in patients at risk (PreSS) compared to age- and gender- matched healthy controls (HC). Patients with primary Sjögren’s syndrome (pSS) showed an even more marked reduction in the naive compartment at the time of diagnosis.
Acknowledgements: NIL.
Disclosure of Interests: None declared.