

Background: The pathogenesis of psoriatic arthritis (PsA) is characterized by a predominant IL-17 signature. Innate-like lymphocytes, such as mucosal-associated invariant T cells (MAIT), are recognized sources of IL-17 in PsA.
To investigate the relevance of MAIT cells, their subsets, and IL-17 production in the synovial fluid (SF) and peripheral blood (PB) of patients with PsA compared to healthy controls (HC), both at baseline and after lymphocyte stimulation.
To evaluate the in vitro effect of tofacitinib and dexamethasone in modulating MAIT cells.
Methods: A case-control study was conducted and PB samples were collected from 10 treatment-naïve patients with PsA, with paired SF in 7 cases. PsA patients had the following characteristics: 5 females (50%), median age 55 years (interquartile range -IQR- 48-58), disease duration 14 months (IQR 6-24), DAPSA 25.5 (IQR 16.3-29.5), serum C-reactive protein 0.21 mg/dL (IQR 0.02-1.93). Two patients had dactylitis, two had enthesitis, none had axial involvement, eight had skin psoriasis, and four had nail psoriasis. PB samples from 6 HC (2 females, 33%; median age 49, IQR 43-54) were used as controls. Mononuclear cells from SF and PB were isolated and analyzed for cell phenotype and IL-17 expression under various conditions, including basal ex vivo conditions and after culture with T cell stimulators [phorbol 12-myristate 13-acetate (PMA) 50 ng/mL and ionomycin (iono) 1 μg/mL], PMA/iono with tofacitinib 300 nM, or PMA/iono with dexamethasone 1000 μM. Levels of IL-17 in the supernatant of SF and PB cultures of PsA patients and HC were also determined with ELISA.
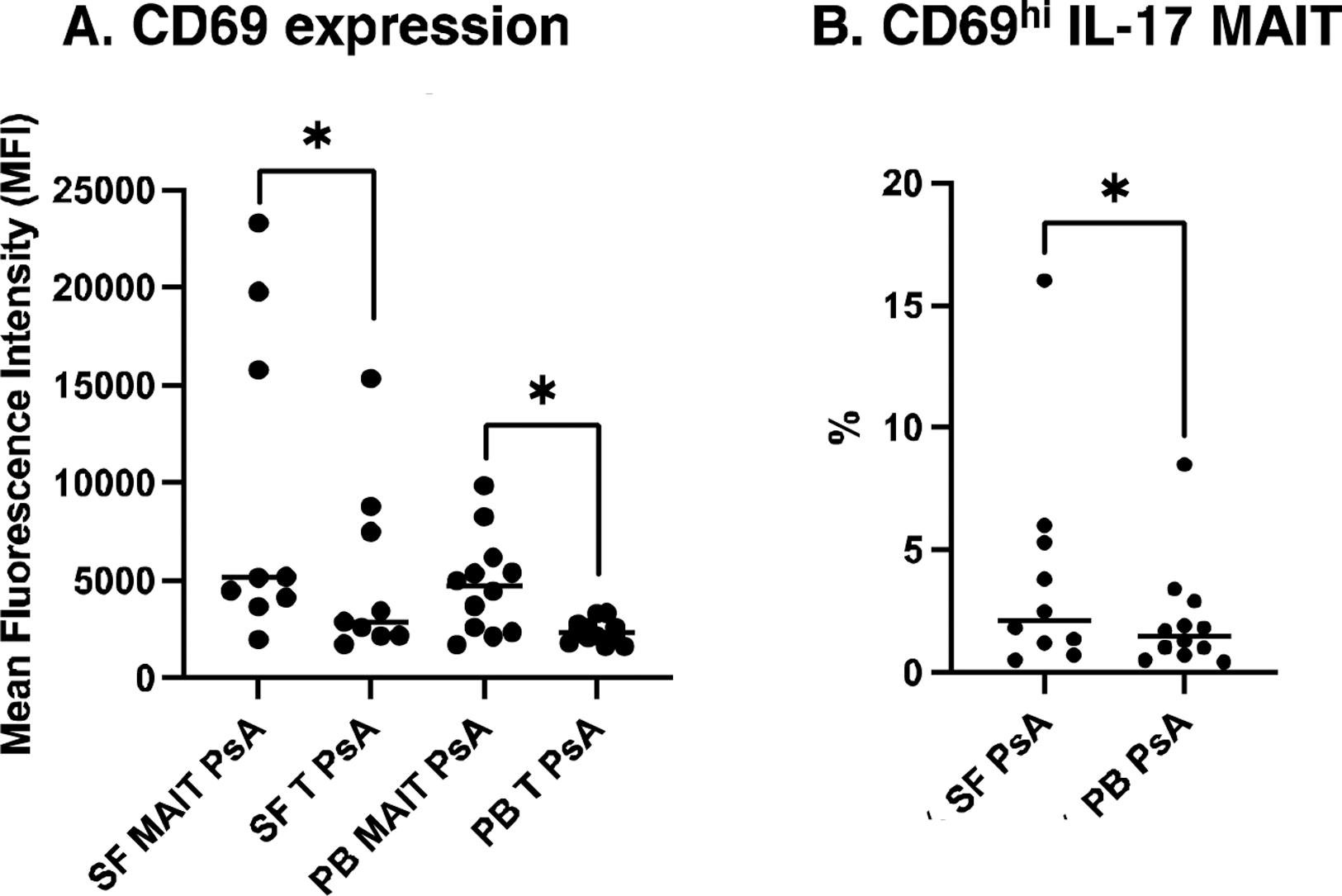
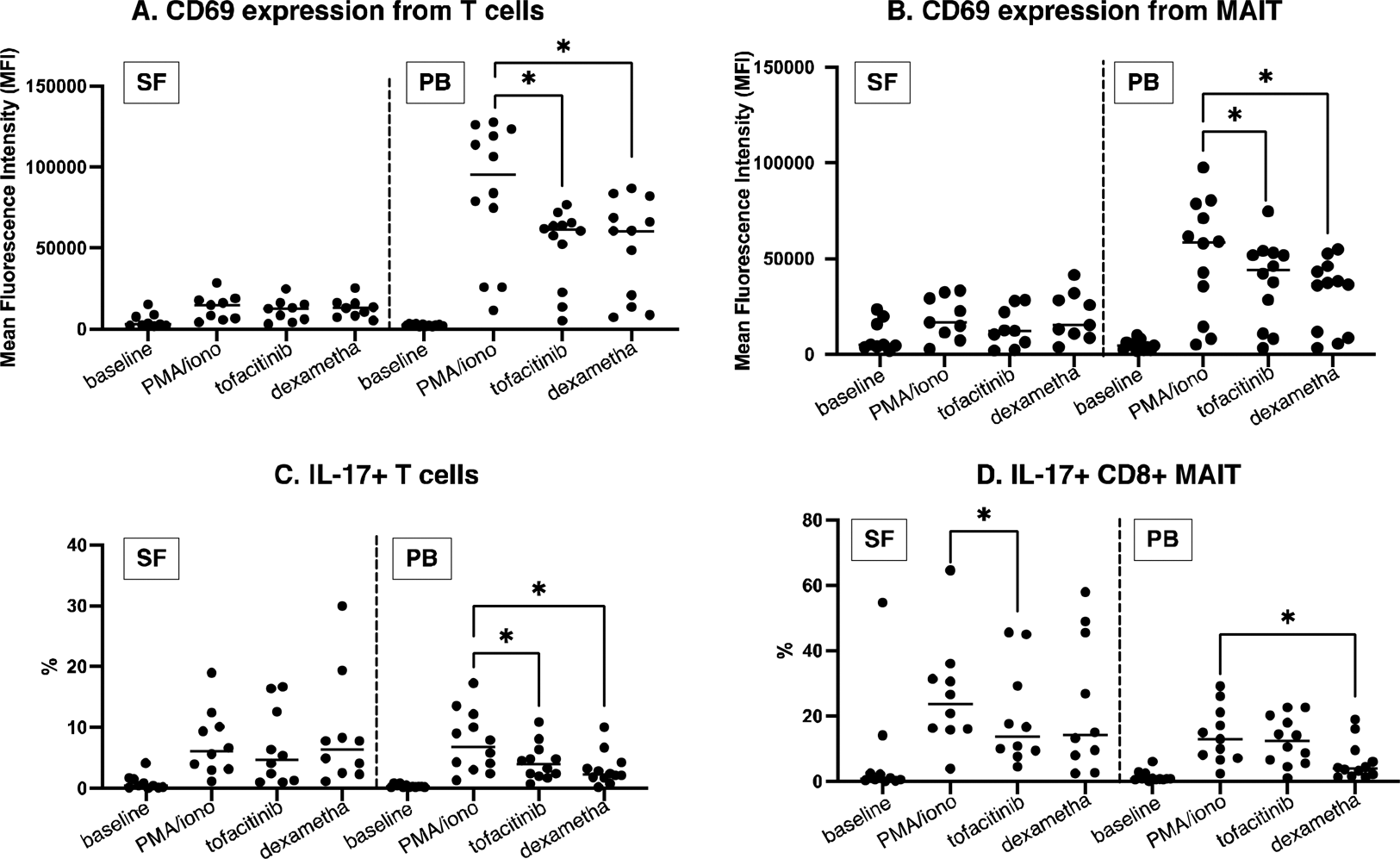
Results: At baseline, the SF of PsA patients was enriched in MAIT cells; moreover, PB T lymphocytes and MAIT cells were more activated in PsA compared to HC, as mirrored by a higher CD69 expression. However, MAIT cells were significantly more activated compared to T cells in both PB and SF (Figure 1A) and in the majority of cases showed a CD8 effector memory phenotype; moreover, activated SF MAIT cells showed the highest percentage of IL17+ cells, compared to PB (Figure 1B). The stimulation with PMA/iono significantly increased CD69 and IL-17 expression, especially in SF-derived PsA cells due to their higher pro-inflammatory prone state. Tofacitinib reduced the expression of CD69 only in PB-derived T lymphocytes and MAIT cells, with a similar magnitude compared to dexamethasone (Figure 2A and B) and significantly reduced PB-derived IL-17+ T lymphocytes and SF-derived IL-17+ MAIT CD8 cells, while dexamethasone had a stronger effect on PB-derived IL-17+ MAIT CD8 (Figure 2, panels C-D). Considering IL-17 levels in culture supernatants, baseline concentrations were higher in PsA SF compared to PB, while PsA PB levels were comparable to controls. Tofacitinib did not significantly reduce the overall IL-17 production compared to dexamethasone.
Conclusion: MAIT cells are enriched in the SF of patients with PsA and display a more activated phenotype with enhanced expression of IL-17. Tofacitinib reduces MAIT cell activation, as well as IL-17 production, in both PsA SF and PB, akin to glucocorticoids but with a more potent effect on MAIT cells.
REFERENCES: NIL.
Comparison between CD69 expression in MAIT and T cells in PsA SF and PB at baseline (panel A); comparison between CD69 hi IL-17-producing MAIT in PsA SF and PB at baseline (panel B).
Modulation of CD69 expression from T cells (panel A) and MAIT (panel B) with tofacitinib and dexamethasone. Modulation of IL-17+ T cells (panel C) and MAIT CD8 (panel D) with tofacitinib and dexamethasone.
Acknowledgements: NIL.
Disclosure of Interests: Maria De Santis: None declared, Antonio Tonutti: None declared, Francesca Motta: None declared, Natasa Isailovic: None declared, Angela Ceribelli: None declared, Giacomo Maria Guidelli AbbVie, BMS, Eli-Lilly, Galapagos, Janssen, Novartis, AbbVie, BMS, Eli-Lilly, Galapagos, Janssen, Novartis, Daniela Renna AbbVie, Eli-Lilly, Janssen, Novartis, AbbVie, Eli-Lilly, Janssen, Novartis, Nicoletta Luciano AbbVie, BMS, Eli-Lilly, Galapagos, Janssen, Novartis, AbbVie, BMS, Eli-Lilly, Galapagos, Janssen, Novartis, Carlo Selmi AbbVie, Amgen, Alfa-Sigma, Biogen, Eli-Lilly, EUSA Pharma - Recordati, Galapagos, Janssen, Novartis, Octapharma, Pfizer, Recordati Rare Disease, SOBI, AbbVie, Amgen, Alfa-Sigma, Biogen, Eli-Lilly, EUSA Pharma - Recordati, Galapagos, Janssen, Novartis, Octapharma, Pfizer, Recordati Rare Disease, SOBI, AbbVie, Amgen, Janssen, Novartis, Pfizer.