

Background: Autoimmunity and immune dysregulation may account for the cardiovascular risk excess in rheumatoid arthritis (RA), although exact mechanisms are incompletely understood. Angiogenic T-cells (Tang) may counteract endothelial damage, by collaborating with endothelial progenitor cells (EPC) in vascular repair. Tang depletion was linked to overt cardiovascular disease in established RA. Whether Tang are disturbed in the early stages of the disease is unknown.
Objectives: To evaluate circulating Tang levels in the earliest stages of arthritis, including clinically suspect arthralgia (CSA), and their associations with subclinical CV endpoints (subclinical atherosclerosis and vascular stiffness).
Methods: 84 untreated RA patients (2010 EULAR/ACR classification criteria; 68% RF, 65% ACPA; mean DAS28: 5.16±1.44), 14 CSA individuals (EULAR definition; 57% RF, 50% ACPA) and 28 matched healthy controls (HC) were recruited. Tang (CD3+CD31+CXCR4+) and EPC (CD34+VEGFR2+CD133+) subsets were assessed by flow cytometry in peripheral blood samples. Plaque occurrence, cIMT and stiffness parameters were analyzed by Doppler ultrasound. Lipoprotein analyses were performed by NMR. Cardiometabolic-related proteins were assessed in serum using high-throughput targeted proteomics.
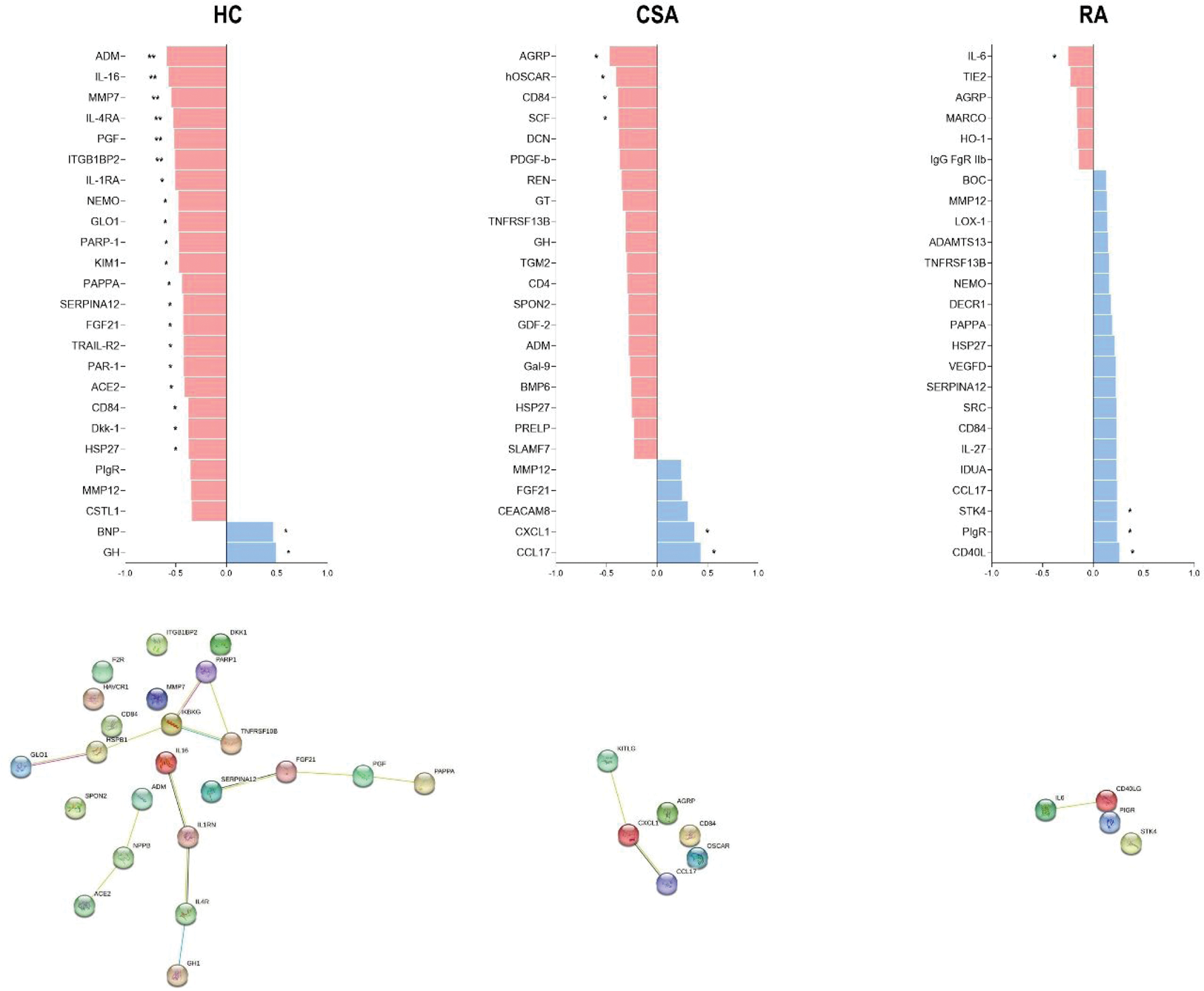
Results: Tang frequency was decreased in arthralgia and RA patients compared to HC (p<0.050 and p<0.001, respectively). Although both CD4+ and CD8+Tang subsets were reduced in RA (p<0.001) compared to HC, only the CD4+Tang subset was diminished in arthralgia (p<0.050). Tang counts paralleled those EPC in HC (r=0.671, p<0.001), but this association was absent in arthralgia (r=0.423, p=0.131) and RA (r=-0.157, p=0.168). Similarly, Tang were negatively correlated with very low density lipoproteins features (cholesterol and triglyceride content, size distribution and particle number) and positively with HDL (cholesterol content and particle number) in HC (all p<0.010), whereas no associations were retrieved in RA and CSA groups. Proteomic analyses revealed that Tang frequency was associated with protein signatures related to blood pressure and vascular tone regulation in HC, whereas associations in RA and CSA were limited and related to inflammatory circuits (Figure 1).
In RA patients, Tang levels were unrelated to traditional risk factors, body mass index or waist circumference (all p>0.050). However, disease activity accounted for Tang depletion both in univariate and multivariate analyses (B [95%CI]; DAS28: -0.121 [-0.193, -0.049], p<0.001; SDAI: -0.013 [-0.022, -0.003], p=0.008; CDAI: -0.014 [-0.024, -0.004], p=0.008). Tang frequency paralleled stiffness parameters: vascular strain (VS: r=0.373, p=0.013), distensibility (VD: r=0.479, p=0.004), stiffness (VSf: r=-0.400, p=0.007) and pressure-strain elastic modulus (PSEM: r=-0.373, p=0.013) in RA. Tang frequency remained as an independent predictor of stiffness parameters after adjusting for confounders (all p<0.050).
Conclusion: Circulating Tang showed (vasculo)-protective associations in healthy controls, which are absent in arthritis. Tang depletion occurs early along RA development, linked to inflammation and disease activity. Circulating Tang may be a biomarker of premature vascular stiffness during the first stages of the disease.
REFERENCES: NIL.
Acknowledgements: ISCIII (PI21/00054, and FI22/00148).
Disclosure of Interests: None declared.