

Background: Dyslipidaemia has been widely reported in rheumatoid arthritis (RA). In non-pregnant patients, metabolomic approaches have led to the discovery of biomarkers for high disease activity and predictors of treatment response. Pregnancy is associated with major changes in lipid metabolism and with an overall ameliorative effect on RA disease activity, followed by postpartum (PP) flare in 50% of patients. The RA metabolome and its relationship with disease activity has not yet been studied in pregnancy.
Objectives: We conducted a prospective pilot study using a 250-metabolite nuclear magnetic resonance (NMR) spectroscopy platform and machine learning (ML) analyses to (1) study metabolic changes in pregnant women with RA in comparison to healthy pregnancy and (2) identify metabolites associated with RA disease amelioration in pregnancy and PP flare.
Methods: Pregnant women with RA (RA-P) and healthy control pregnant women (HC-P) were assessed at <13 weeks (T1), 13–27 weeks (T2), >28 weeks (T3), and within 6 months PP. RA disease activity was measured with DAS28(3)CRP, which is recommended in pregnancy. Disease amelioration in pregnancy was assessed using ΔDAS pre-preg–T3 , calculated as: DAS28(3)CRP in T3 – DAS28(3)CRP within 6 months pre-pregnancy (obtained from patient records). PP flare was assessed using ΔDAS T3–PP , calculated as: DAS28(3)CRP in PP – DAS28(3)CRP in T3. Age-matched (± 5 years) controls were recruited: non-pregnant women with RA (RA-NP)and healthy control non-pregnant women (HC-NP), both at a single timepoint. Serum was collected from all participants and analysed using NMR spectroscopy. The data were analysed using supervised ML algorithms in appropriate software.
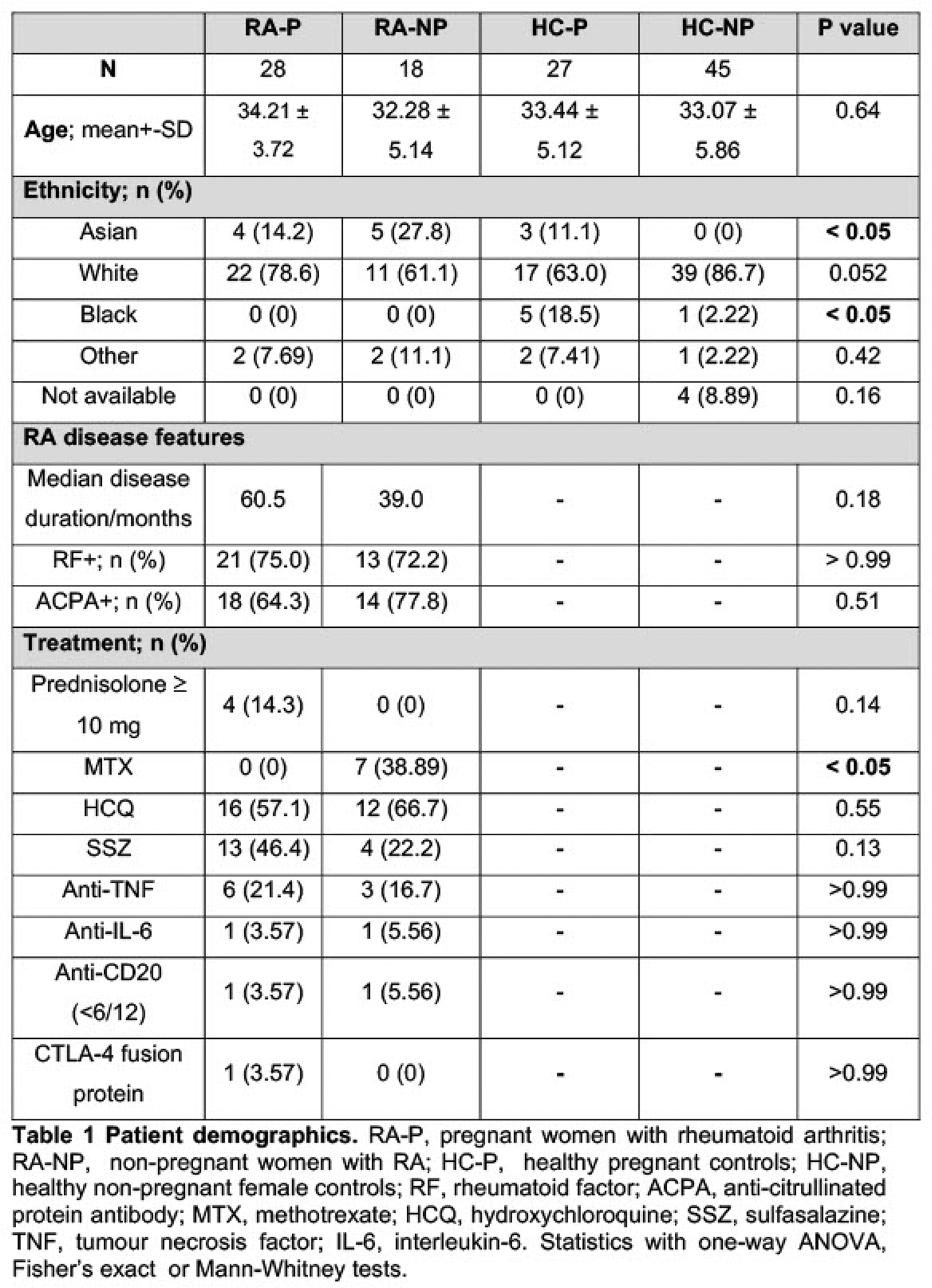
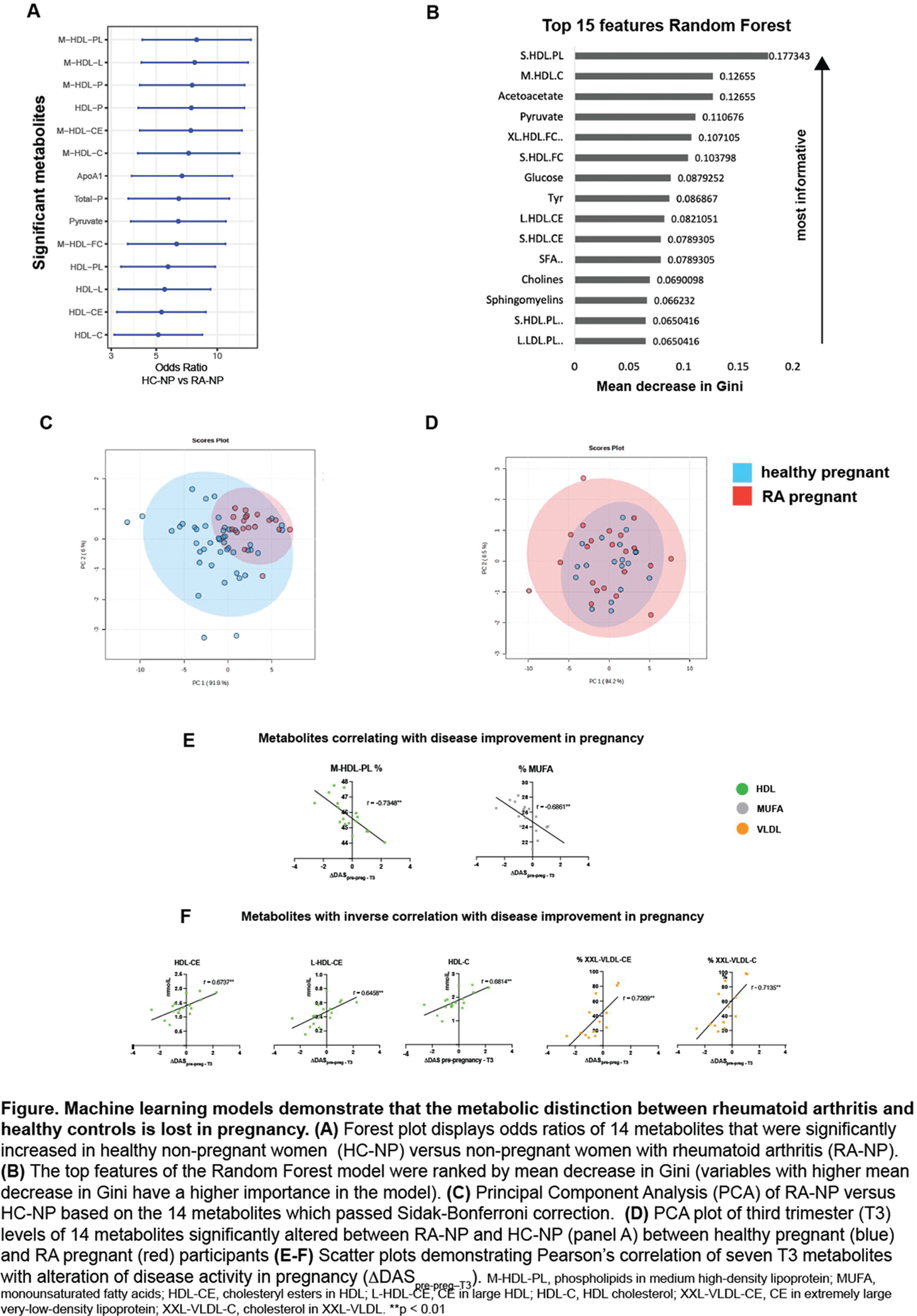
Results: N=118 subjects were recruited: 28 RA-P; 18 RA-NP; 27 HC-P; and 45 HC-NP. Demographic and clinical features are shown in Table 1. Patients (n=3 in T3) on prednisolone ≥10 mg/day were excluded. Median DAS28(3)CRP scores were consistent with low disease activity/remission in both RA groups/timepoints: RA-NP, 2.54 (95% CI [1.94, 3.14]); RA-P T3, 2.20 [1.84, 2.56]; RA-PP 2.61 [1.91, 3.30]. Mean ΔDAS pre-preg–T3 was -0.53 [-1.09, 0.04] and mean ΔDAS T3–PP was 0.33 [-0.24, 0.90]. Multiple t tests followed by Bonferroni correction found 14 metabolites that were significantly reduced in RA-NP vs HC-NP, of which 11 were HDL-related (Figure 1A). Three supervised binary classification ML methods were employed to assess whether RA patients could be predicted from HC based on metabolic profile alone. The Random Forrest model had the highest area under the curve (0.737) and identified S-HDL-PL, M-HDL-C, and acetoacetate as the three most informative metabolites (Figure 1B). In both HC-P and RA-P there were marked increases in lipoprotein and lipid metabolites, particularly very-low-density lipoprotein. Longitudinal comparisons showed that T3 was the peak of metabolic change in both groups. Comparisons of HC-P and RA-P and PP found no significant metabolite differences (false discovery rate=5%) at T2, T3 or PP (multiple unpaired t tests). Principal component analysis of the 14 metabolites that distinguished non-pregnant RA from HC (Figure 1C) found no such distinction in pregnancy (Figure 1D). Pearson’s correlation of ΔDAS pre-preg–T3 with T3 metabolite levels found seven significantly correlated metabolites (p<0.01) . M-HDL-PL% and MUFA% correlated negatively with ΔDAS pre-preg–T3 (improving disease activity in pregnancy), while L-HDL-CE, HDL-CE, HDL-C, XXL-VLDL-CE% and XXL-VLDL-C% correlated positively with ΔDAS pre-preg–T3 (increasing disease activity in pregnancy) (Figure 1E-F). Metabolic associations of postpartum flare were assessed by correlating T3 metabolite levels with ΔDAS T3–PP . Glutamine, albumin and six HDL-related metabolites were inversely correlated with ΔDAS T3–PP (reduced at T3 in patients who subsequently flared in PP), p<0.05.
ML methods identified RA patients from HC based on serum metabolite profile (mainly HDL deficiency) in non-pregnancy.
The metabolic distinction between RA and HC is lost in pregnancy.
We have identified metabolites associated with amelioration/flare of RA in pregnancy and with PP flare.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Charles Raine UCB Investigator Initiated Studies grant, Isabella Sheldon: None declared, George Robinson: None declared, Junjie Peng: None declared, Coziana Ciurtin: None declared, Jessica Manson: None declared, David Williams: None declared, Elizabeth Jury: None declared, Ian Giles UCB, UCB.