

Background: Axial Spondyloarthritis (AxSpA) and axial Psoriatic Arthritis (AxPsA) have overlapping features but also meaningful differences in genetics, clinical presentation and immunophenotype. Active sacroiliitis may be evident in both entities through bone marrow oedema (BME) on magnetic resonance imaging (MRI). Radiomics emerged as a new frontier in the Rheumatology landscape [1]. Its roots are in oncology, where it has primarily demonstrated its importance in diagnostic and therapeutic prediction. Radiomics involves extracting and analyzing many quantitative features from medical images, including shape, intensity, texture, and spatial relationships, converting imaging into high-dimensional data correlating with tissue histopathology, and mimicking a digital biopsy.
Objectives: To investigate whether the radiomic features of sacroiliac joints BME may help to discriminate AxSpA from AxPsA.
Methods: Our analysis included patients with classified AxSpA according to Assessment of SpondyloArthritis International Society (ASAS) criteria and those with classified PsA according to CAPSAR criteria and axial involvement who underwent MRI scans with a magnetic field > 1 Tesla who underwent MRI scans with a magnetic field > 1 Tesla between January 1
st
2018 and December 31
th
2022 at our centre. To be enrolled, patients had to exhibit active sacroiliitis, as defined by ASAS [2]. BME was manually segmented by an expert radiologist on axial scans in a short tau inversion recovery (STIR) sequence using 3D Slicer ver 5.2.1 (Sample video:
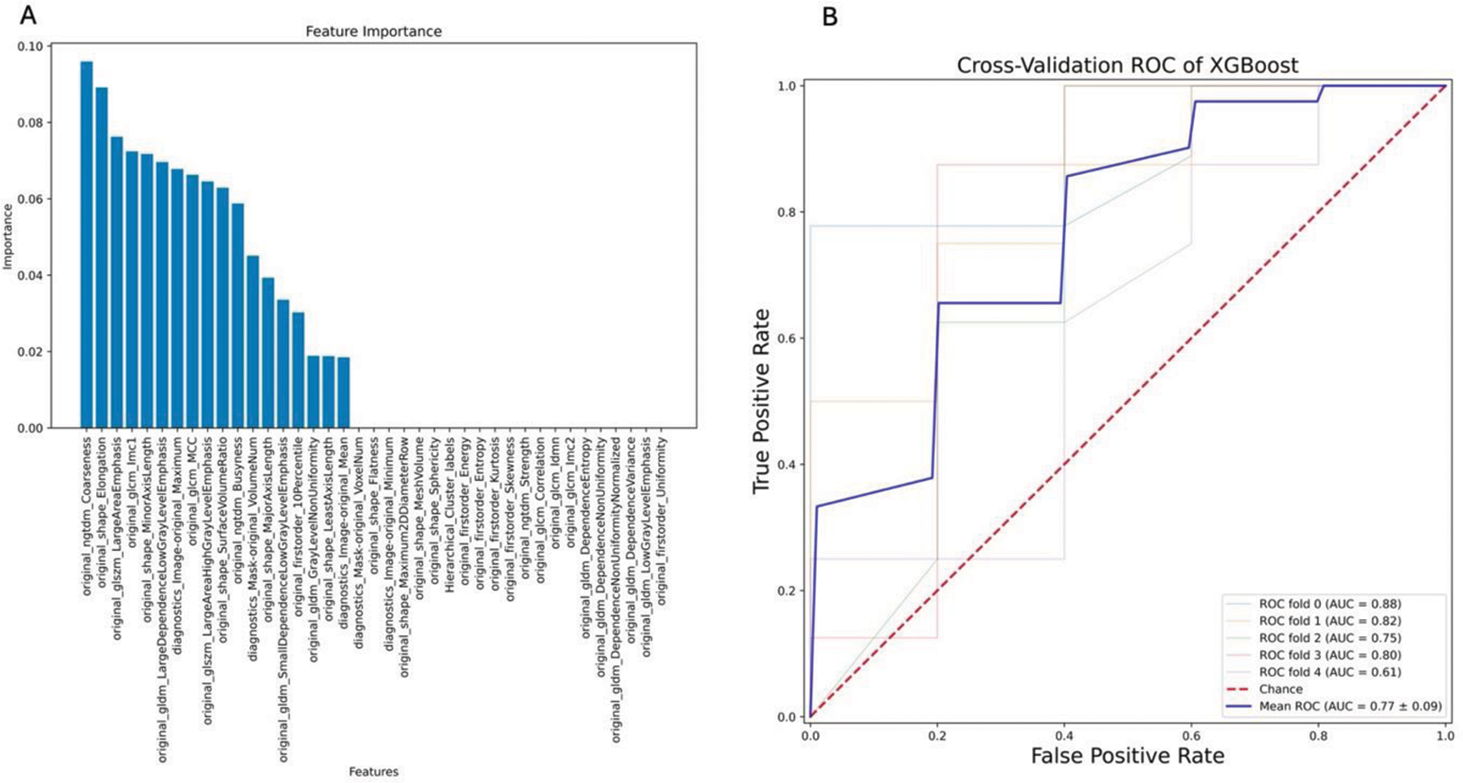
Results: We enrolled n.66 patients, 41/66 (62.12%) with AxSpA and 25/66 (27,88%) with AxPsA. Those with AxSpA mainly were female (28/41, 68.29%) with mean age ± SD of 41.09 ± 15.27 years and mean disease duration 69.85 ± 68.63. The mean ASDAS-CRP was 2.69 ± 0.97. AxPsA patients (female 14/25, 56%) had a mean age of 45.08 ± 11.73 years and a mean disease duration of 74.16 ± 66.70 months, whereas ASDAS-CRP was 2.87 ± 0.80. After checking for autocorrelation, only 39 features were retained. Based on that, XGBoost could predict correct diagnosis with an Accuracy of 0.80 ± 0.07, Precision 0.86 ± 0.10, Recall 0.86 ± 0.10 and AUROC 0.77 ± 0.09 (Figure 1 B)
XGBoost showed that the most important features for prediction were components of:
The texture of the BME ( original_ngtdm_Coarseness, original_glcm_Imc1),
The shape of the BME ( original_shape_Elongation, original_shape_MinorAxisLength ) and
The grey level intensity of the BME ( original_glszm_LargeAreaEmphasis, original_glszm_LargeAreaHighGrayLevelEmphasis ),
as depicted in Figure 1 A.
Conclusion: The radiomic features of segmented BME can help discriminate between AxSpA and AxPsA. Because the texture and grey level zones of BME are so crucial for the forecast, one may speculate that the osteitis itself may differ between such diseases, not only because of extent and laterality.
Further research is needed to externally validate such an approach, checking for potential confounders.
REFERENCES: [1] Venerito V et al. Front Med (2023). 9:1069486.
[2] Lambert RG et al. Ann Rheum Dis. 2016 Nov;75(11):1958-1963.
Acknowledgements: NIL.
Disclosure of Interests: None declared.