

Background: Recently, monosodium urate (MSU) deposits were demonstrated in coronary arteries of 86.4% of gout patients by dual energy computed tomography (DECT).[1] Cardiovascular (CV) MSU deposits were associated with major adverse cardiac events (MACE) [2], but also the presence of peripheral MSU deposits increased the risk for CV disease and death.[3]
Objectives: The aim of this retrospective analysis was to evaluate the possible association of 1) peripheral MSU deposits with CV MSU deposits and 2) the presence of MSU deposits with MACE.
Methods: We included all patients, recruited at the radiology department of medical university Innsbruck with clinically or ultrasound-based suspicion of gout, who performed ultrasound and DECT of the affected limb as well as of the thorax between 01.05.2012 and 01.09.2019. Clinical and laboratory parameters were retrieved from patients´ charts. Gout was defined according to the ACR/EULAR classification criteria, uric acid levels over 6 mg/dl or ongoing uric acid lowering treatment without clinical signs of gout specified hyperuricemia patients and control group definition was achieved when uric acid levels were normal without concomitant uric acid lowering therapy and absence of gout symptoms. Peripheral MSU deposits and tophi were identified using DECT. A tophus was arbitrarily defined as MSU deposit >1cm diameter. If present, the maximum diameter of the tophus was measured. Medical history review identified the presence of MACE, defined as myocardial infarction and/or stroke. For statistical appraisal, χ 2 statistic based on a 2 × 2 tabulation, and Mann–Whitney U tests were performed using IBM SPSS (version 27). P < 0.05 was used as the cut-off for statistical significance.
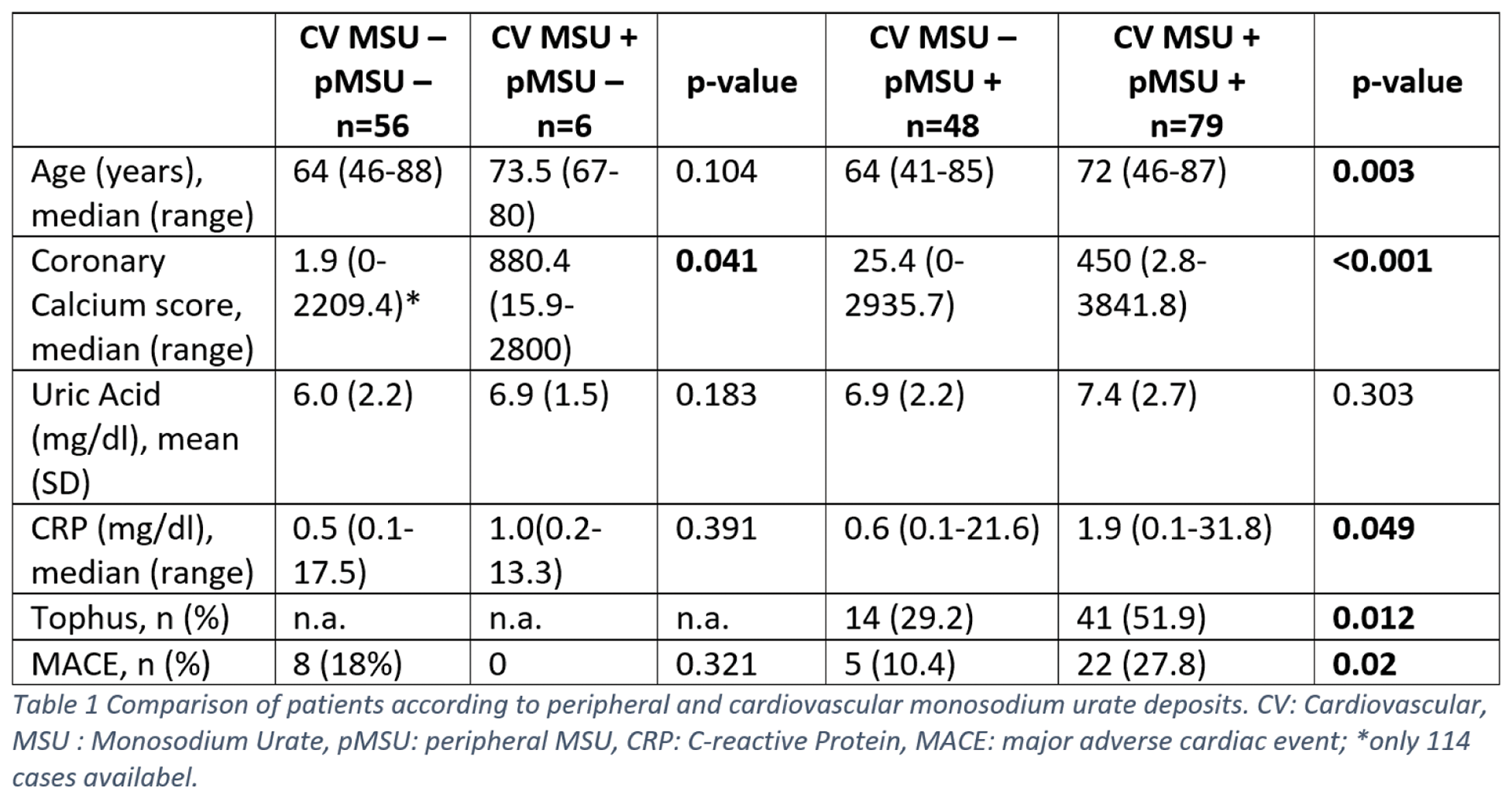
Results: Out of the 189 patients recruited, peripheral MSU deposits were present in 126 (66.7%) cases. 103 (103/131, 78.6%) were gout patients and 23 (23/40, 57.5%) were hyperuricemia patients. Of those 126, 55 patients (50 gout, 5 hyperuricemia patients) were tophaceous. Median peripheral tophus size was 2 cm (range 1-8cm). 62.7% (n=79) of our patients with peripheral MSU deposits revealed CV MSU positive plaques (61 gout, 18 hyperuricemia patients). Tophaceous patients showed higher serum uric acid levels [mean 7.8 (SD 2.7) vs 6.5 (SD 2.2) mg/dl, p=0.002] but inflammatory parameters [C-reactive protein (CRP): median 1.5 (range 0.1-25.2) vs 0.6 (range 0.1-31.8), p=0.095] were equally distributed in tophaceous and non-tophaceous patients. When comparing age, coronary calcium score, uric acid, CRP, presence of tophi and MACE between patients with and without peripheral and CV MSU deposits, significant differences were shown in age, coronary calcium score, CRP-levels as well as tophi and MACE (see Table 1). Both, non-tophaceous peripheral MSU deposits as well as tophi were associated with CV MSU deposits (p<0.001, respectively). Only tophi, but not peripheral MSU deposits, were associated with the presence of MACE (p=0.047). Overall 35 MACE occurred, in tophaceous patients 15 MACE (27.3%) were documented. Tophus size/diameter showed no difference in patients with MACE [median 2cm (range 1-5)] when compared to those without MACE [median 2cm (range 1-8cm), p=0.933].
Conclusion: To our knowledge, this is the first study demonstrating the association of peripheral MSU deposits and tophi with the presence of CV MSU plaques. MACE was more prevalent in patients with peripheral tophaceous MSU deposits. In contrast to previous published data, peripheral tophus size was not related to the occurrence of MACE in our cohort.
REFERENCES: [1] Klauser, A.S., et al., Dual-Energy Computed Tomography Detection of Cardiovascular Monosodium Urate Deposits in Patients With Gout. JAMA Cardiol, 2019.
[2] Held, J., et al., OP0155 CLINICAL IMPACT OF CARDIOVASCULAR MONOSODIUM URATE DEPOSITS MEASURED BY DUAL ENERGY COMPUTED TOMOGRAPHY: A RETROSPECTIVE EVALUATION. Annals of the Rheumatic Diseases, 2023. 82 (Suppl 1): p. 102-103.
[3] Marty-Ané, A., et al., Crystal deposition measured with dual-energy computed tomography: association with mortality and cardiovascular risks in gout. Rheumatology (Oxford), 2021. 60 (10): p. 4855-4860.
Acknowledgements: NIL.
Disclosure of Interests: None declared.