

Background: Rheumatoid arthritis (RA) patients have an increased risk of subclinical cardiovascular (CV) disease and, consequently, a higher incidence of CV events, compared to the general population. Coronary artery calcium (CAC) measurement has been shown to be able to predict CV events in the non-RA population. Until today, no studies have assessed how coronary CAC values evolve prospectively in patients with RA and which are the factors associated with CAC changes overtime.
Objectives: To determine how CAC values evolve prospectively in a population of RA patients and which are the factors associated with RA progression.
Methods: Prospective longitudinal study of 95 RA patients without previous CV events who were recruited in 2011. Multidetector computed axial tomography (MCT) was used to assess CAC (Agatston score) levels at baseline and after a mean follow-up time of 5 years. Progression was considered if the second CAC had any value higher than baseline. Multivariate logistic regression was performed to analyze which baseline factors were associated with progression of CAC values.
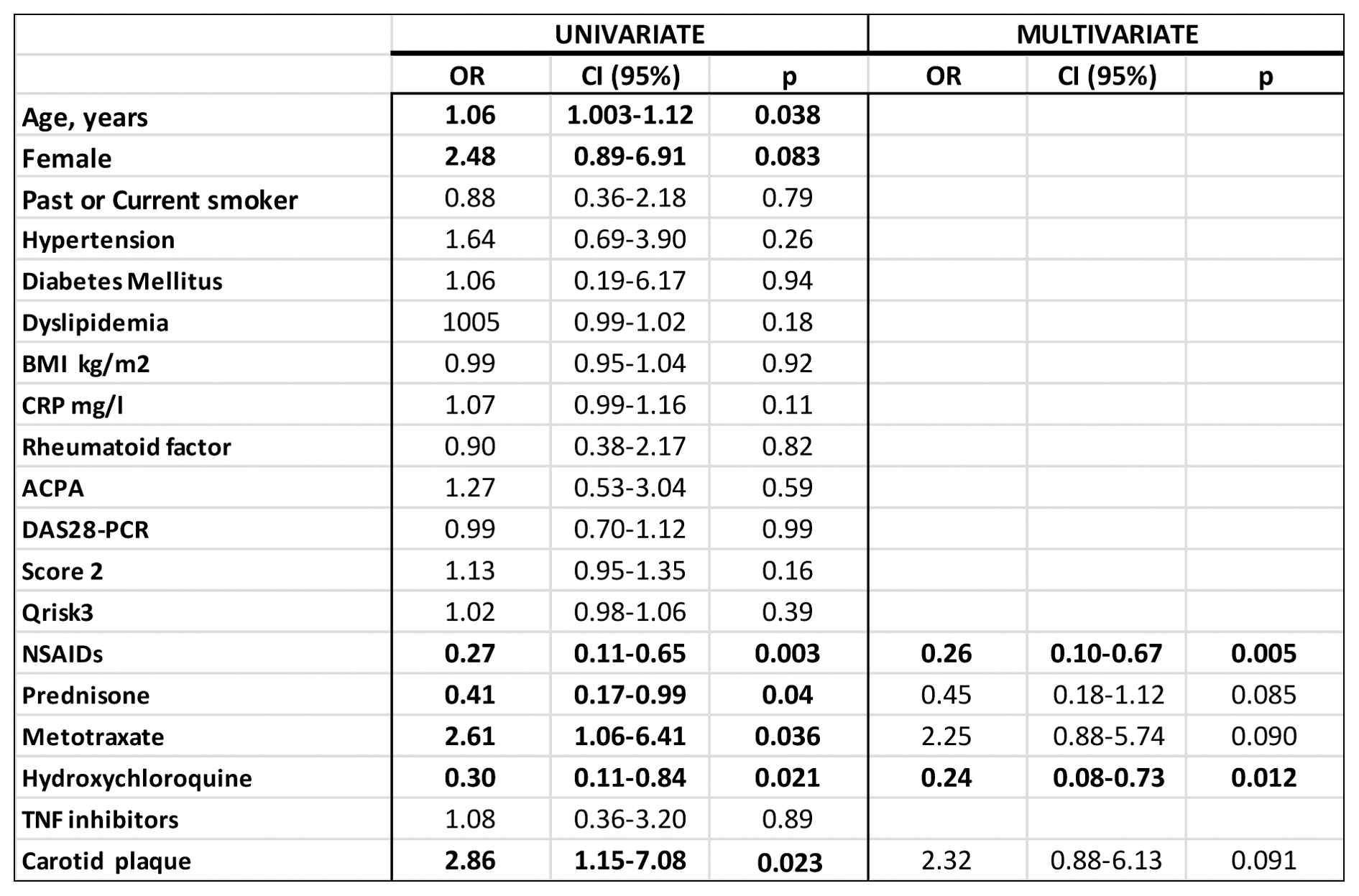
Results: After a mean follow-up time of 5.5 ± 0.4 years, 62 patients (65%) had an increase in CAC, while 33 (35%) had no progression. The main general characteristics, CV risk factors, RA disease activity data and current treatment at baseline are summarized in the Table 1. Age at baseline showed a significant and positive association with an increase in CAC (OR 1.06 [95%CI 1.003-1.12), p=0.038). Similarly, male patients (OR 2.48 [95%CI 0.89-6.91], p=0.083), disclosed a positive relation to CAC augmentation, although, in this case, statistical significance was not reached (Table 2). The presence of classical CV risk factors at baseline showed no significant associations with CAC worsening. This was also the case for baseline levels of lipid profile molecules such as total cholesterol, triglycerides or high- and low-density molecules. Regarding disease-related data, the presence of rheumatoid factor or anti-citrullinated peptide antibody, as well as, baseline levels of glomerular sedimentation rate and C-reactive protein were not associated with changes in CAC value after 5.5 years. In addition, the CV risk indices SCORE2 and QRISK3 showed no ability for the prediction of an increase in CAC values. Besides, after multivariable adjustment, the use of NSAIDs (OR 0.26 [95%CI 0.10-0.67], p=0.005) and hydroxychloroquine (OR 0.24 [95%CI 0.08-0.73], p=0.012) at baseline were associated with a lower risk of increased CAC. No association was found between baseline use of other therapies and changes in CAC overtime. The presence of carotid plaque at baseline showed a significant univariate association with increased CAC. However, after adjustment for covariates this significance was lost although a positive trend was observed (OR 2.32 [95%CI 0.88-6.13], p=0.091).
Conclusion: Sixty-five per cent of patients with RA increase their CAC value after a mean follow-up of 5.5 years. Classical CV risk indices do not predict this worsening of CAC. The use of NSAIDs and hydroxychloroquine are associated with a lower risk of increased CAC. The presence of carotid plaque could be a marker of CAC progression in this population.
REFERENCES: NIL.
TABLE 1. BASELINE CHARACTERISTICS OF 95 ARTHRITIS PATIENTS WITHOUT PREVIOUS CARDIOVASCULAR EVENTS
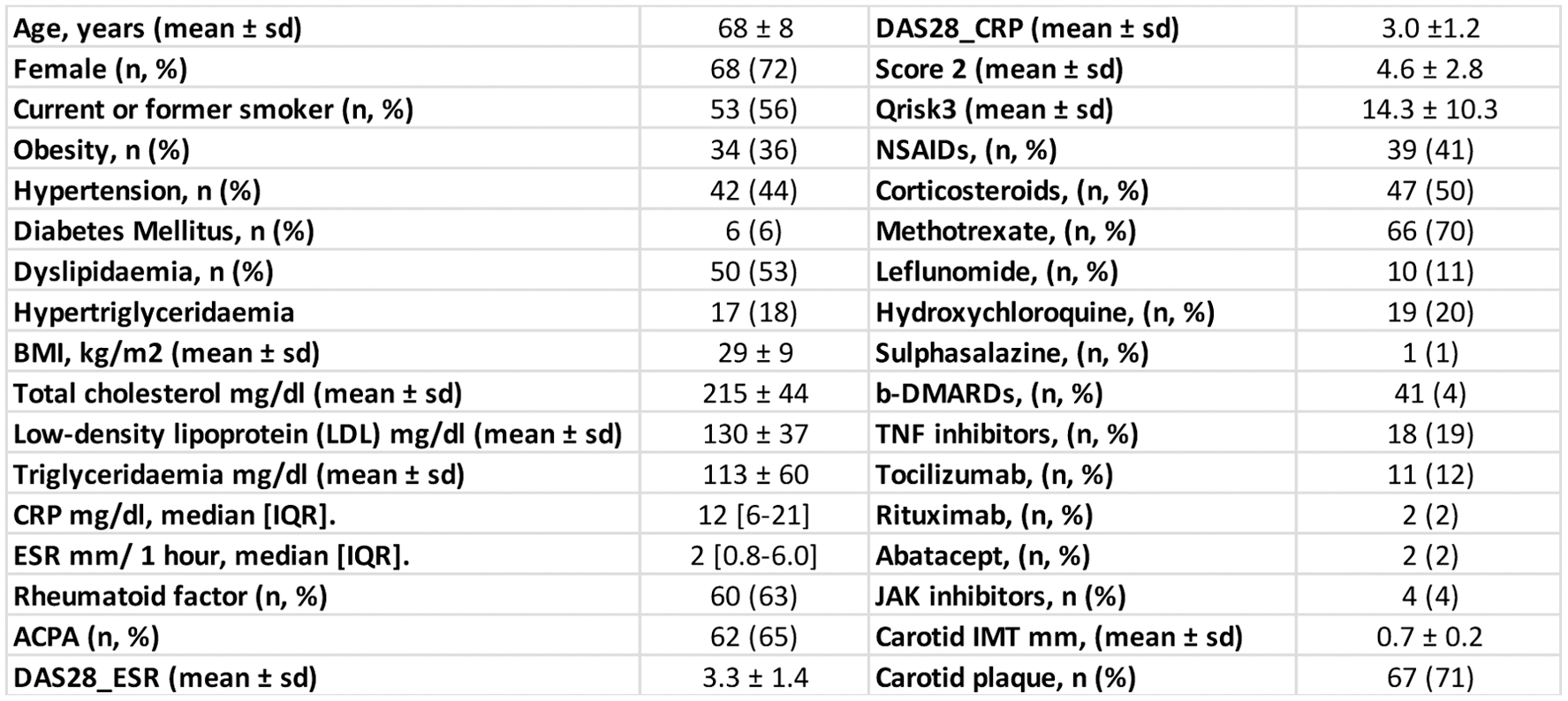
TABLE 2. CORONARY CALCIUM INCREASE. LOGISTIC REGRESSION. MULTIVARIATE ANALYSIS ADJUSTED FOR AGE AND SEX.
Acknowledgements: NIL.
Disclosure of Interests: None declared.