

Background: Rheumatoid arthritis (RA) demands early diagnosis and treatment to prevent joint damage and disability. Presently, diagnosis relies on a combination of clinical evaluation, imaging, and blood tests, which can be costly, time-consuming, and invasive. An emerging new technology is using exhaled breath analysis for the diagnosis of various diseases, including RA. Volatile organic compounds (VOCs) present in breath reflect (patho)physiological processes in the body. VOCs create a unique breath profile that can be analysed to identify patterns. The electronic nose is a handheld electronic device that can measure these VOC breath patterns. Interaction of VOCs with metal-oxide sensors inside the electronic nose result in conductivity changes which can be analysed and recognised using machine learning algorithms.
Objectives: To create a prediction model based on volatile organic compounds in exhaled breath to differentiate between patients with rheumatoid arthritis and non-rheumatoid arthritis controls.
Methods: A prospective, observational, single centre study was conducted at Medisch Spectrum Twente, Enschede, the Netherlands between June 2021 and March 2023. Breath samples were collected from 223 consecutive RA patients and 215 non-rheumatoid arthritis controls. Subjects were instructed to inhale and exhale through the disposable mouthpiece of the electronic nose for five minutes. First, a prediction model was developed using a training set of 338 samples, after which a blinded set of a further 100 samples was used for validation of the model. Machine learning algorithms were employed to process the breath data. The analysis included data normalisation and compression, followed by classifier training, which resulted in operating characteristic curves and related scatter plots.
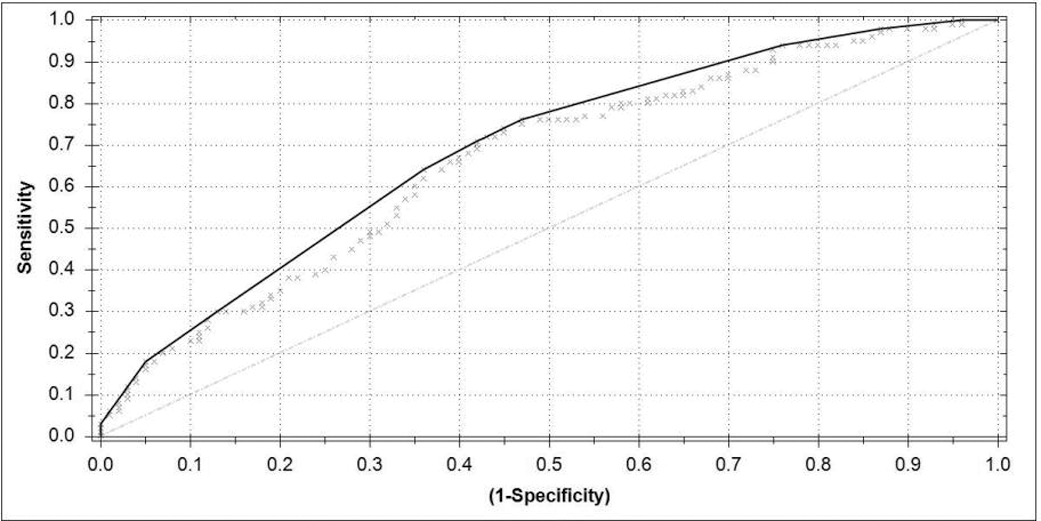
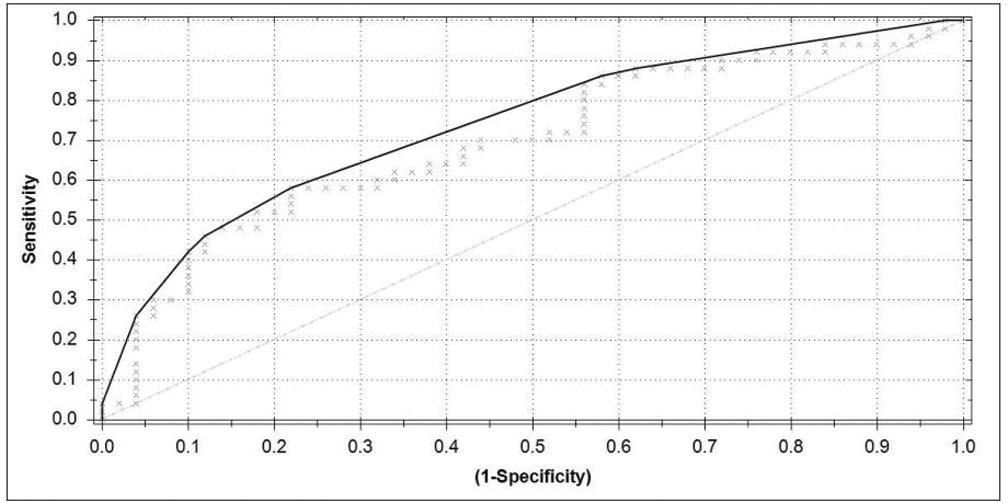
Results: In differentiating between RA and control subjects, the model revealed a moderate discriminatory ability with an ROC AUC of 0.66 for the training set. This set displayed a sensitivity of 0.72, specificity of 057, PPV of 0.64 and NPV of 0.66. The analysis of the blinded set demonstrated performance consistent with the training set, yielding an AUC of 0.70 with a sensitivity of 0.72, a specificity of 0.48, a PPV of 0.58 and a NPV of 0.63.
Conclusion: This study demonstrates the possibility of analysing VOCs to effectively differentiate between patients with RA and controls without RA. These results suggest that use of breath analysis as a screening tool might be useful for more efficient and faster referral to a rheumatologist. Future research is needed to further improve the model by adding clinical parameters to the exhaled-breath data.
REFERENCES: [1] Kort, S., Tiggeloven, M. M., Brusse-Keizer, M., Gerritsen, J. W., Schouwink, J. H., Citgez, E.,... & van der Palen, J. (2018). Multi-centre prospective study on diagnosing subtypes of lung cancer by exhaled-breath analysis. Lung Cancer , 125 , 223-229.
[2] Kort, S., Brusse-Keizer, M., Gerritsen, J. W., Schouwink, H., Citgez, E., de Jongh, F.,... & van der Palen, J. (2020). Improving lung cancer diagnosis by combining exhaled-breath data and clinical parameters. ERJ open research , 6 (1).
. The electronic nose device

. ROC curve from the analysis of the training set differentiating between RA and non-RA patients.
. ROC curve from the analysis of the blind set differentiating between RA and non-RA patients.
Acknowledgements: NIL.
Disclosure of Interests: Demy Gerritsen: None declared, Ruben Scheps: None declared, Chris Blaauwgeers: None declared, Mirjam Hegeman: None declared, Peter ten Klooster: None declared, Harald E. Vonkeman AbbVie, Novartis, Pfizer, UCB, Johnson and Johnson, Galapagos, Boehringer Ingelheim.