

Background: Despite improved clinical outcomes for rheumatoid arthritis (RA), a considerable proportion of patients with the disease continue to experience treatment failure. In such cases, patients and rheumatologists may experience multiple trial-and-error treatment attempts before remission or induction of low disease activity. Regarding the uncertainty in selecting biologic agents or Janus kinase inhibitors (JAKi) with differing mechanisms of action, predicting which patients with RA would respond to treatment would enable rapid achievement of treatment targets.
Objectives: This study aimed to predict treatment response to anti-tumor necrosis factor (anti-TNF) and JAKi therapies in patients with RA via machine learning (ML).
Methods: Patients with RA and moderate or high disease activity, who had started on anti-TNF or JAKi therapy, were identified from the prospective observational Korean College of Rheumatology Biologics and targeted therapy (i.e., “KOBIO”) registry. This registry houses data for patients ≥ 18 years of age who had undergone anti-TNF (n=574) or JAKi (n=209) therapies for ≥ 1 year. Among the ML models, extreme gradient boosting (XGBoost) was used to predict the initial treatment response within a year. The following variables at baseline were included for developing the predictive models: demographic information; autoantibodies; erythrocyte sedimentation rate and C-reactive protein level; Disease Activity Score in 28 joints (DAS 28); Simplified and Clinical Disease Activity Index (SDAI, CDAI, respectively); disease-modifying antirheumatic drugs; and glucocorticoids. Treatment response was defined as achieving low disease activity or remission as measured by the DAS28-ESR within the first 6-12 months after initiation of anti-TNF or JAKi therapy. The ML models were trained using 5-fold cross validation and features were selected via the sequential forward method.
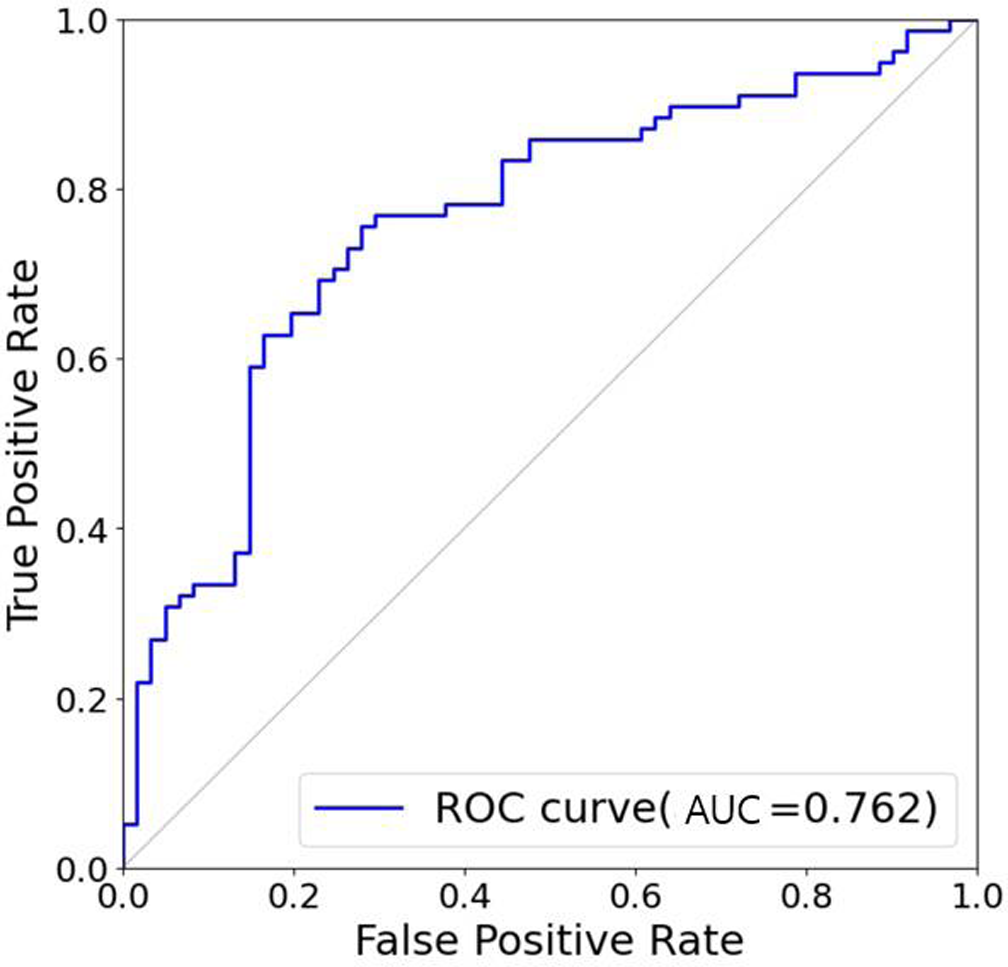
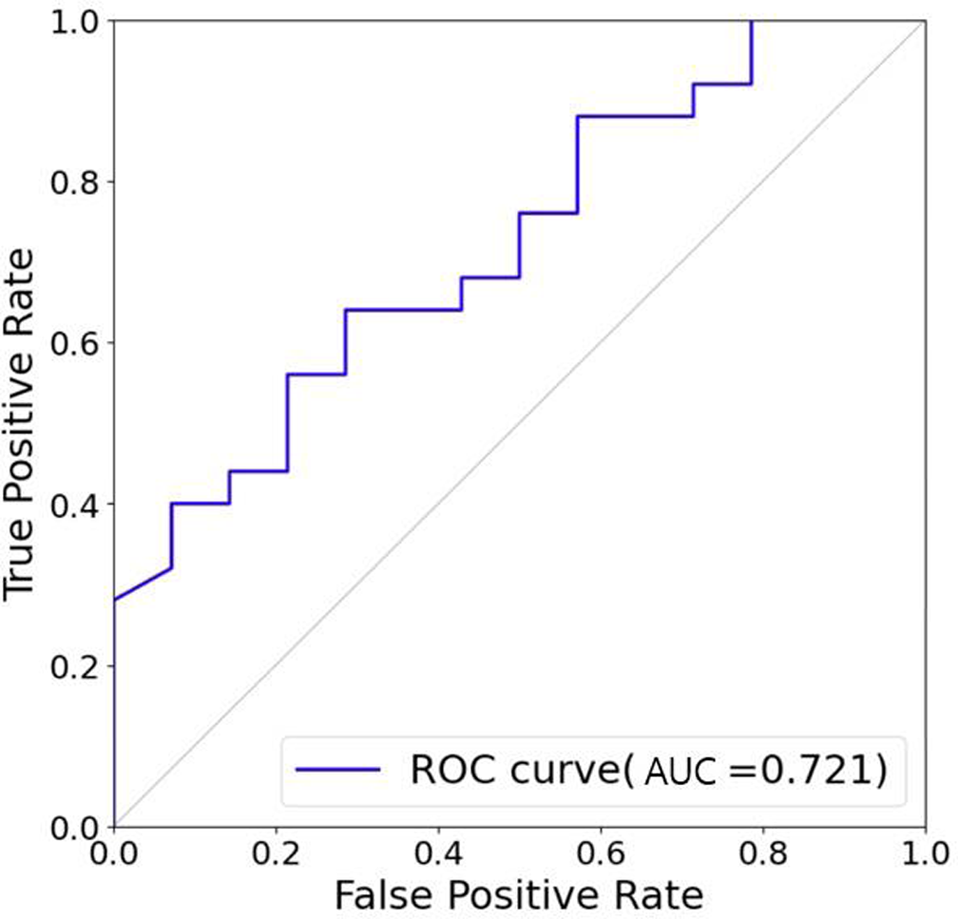
Results: The overall response rates for anti-TNF and JAKi therapies were 56 and 64%, respectively. Among the ML models, XGBoost achieved the highest predictive accuracies with the area under the receiver operating characteristics curve (ROC-AUC) of 0.762 and 0.721 for the two, respectively. The seven most important features in these models included SDAI, current smoking, glucocorticoid, and patient global health.
Conclusion: ML provided an accurate prediction of treatment response to anti-TNF or JAKi in patients with RA. These findings may lead to the development of personalized treatment strategies and improve clinical effectiveness by reducing treatment failure for RA.
REFERENCES: [1] Norgeot B, Glickberg BS, Trupin L, Lituiev D, Gianfrancesco M, Oskotsky B, et al. Assessment of a deep learning model based on electronic health record data to forecast clinical outcomes in patients with rheumatoid arthritis. JAMA Netw Open 2019;2:e190606.
[2] Matsuo H, Kamada M, Imamura A, Shimizu M, Inagaki M, Tsuji Y, et al. Machine learning-based prediction of relapse in rheumatoid arthritis patients using data on ultrasound examination and blood test. Sci Rep 2022;12:7224.
Key words: Machine learning, anti-tumor necrosis factor, Janus kinase inhibitor, rheumatoid arthritis,
Figure 1. ROC curves for predicting treatment response in patients with RA.
ROC curves for XGboost for predicting treatment response in RA patients treatment with anti-tumor necrosis factor (anti-TNF) (A), and Janus kinase inhibitor (JAKi) (B). ROC, receiver operating characteristics; AUC, area under the ROC curve: RA, rheumatoid arthritis.
Acknowledgements: We thank the Korean College of the Rheumatology for access to the data registry.
Disclosure of interest: None declared.
Acknowledgements: We thank the Korean College of the Rheumatology for access to the data registry.
Disclosure of Interests: None declared.