

Background: The Sydney criteria were the classification criteria for antiphospholipid syndrome (APS) used until 2023. They included a clinical domain (vascular thrombosis or pregnancy morbidity) and an analytical domain (positivity of anticardiolipin antibodies [aCL], anti-beta2 glycoprotein [aB2GP1] and lupus anticoagulant [AL]). However, multiple studies have shown that there is large clinical and analytical variability within these patients. With the objective of better classifying these patients, in 2023 the American College of Rheumatology (ACR)/ Alliance of Associations for Rheumatology (EULAR) published the new APS classification criteria. These included other clinical criteria, previously called non-criteria manifestations, which include microvascular, haematological or cardiac manifestations, previously considered less frequent or atypical.
Objectives: To analyse whether the non-criteria manifestations differ in frequency between triple positive APS (APS-TP) and non-triple positive APS patients (nTP-APS). To compare the cardiac manifestations between patients with APS-TP and APS-nTP.
Methods: Observational transversal study with a cohort of patients from a tertiary care hospital. Patients needed to have a diagnosis of APS and any of the clinical manifestations included in the new ACR/ EULAR classification of 2023. Sociodemographic, clinical and analytical (aCL, aB2GP1 and AL) variables were analysed.
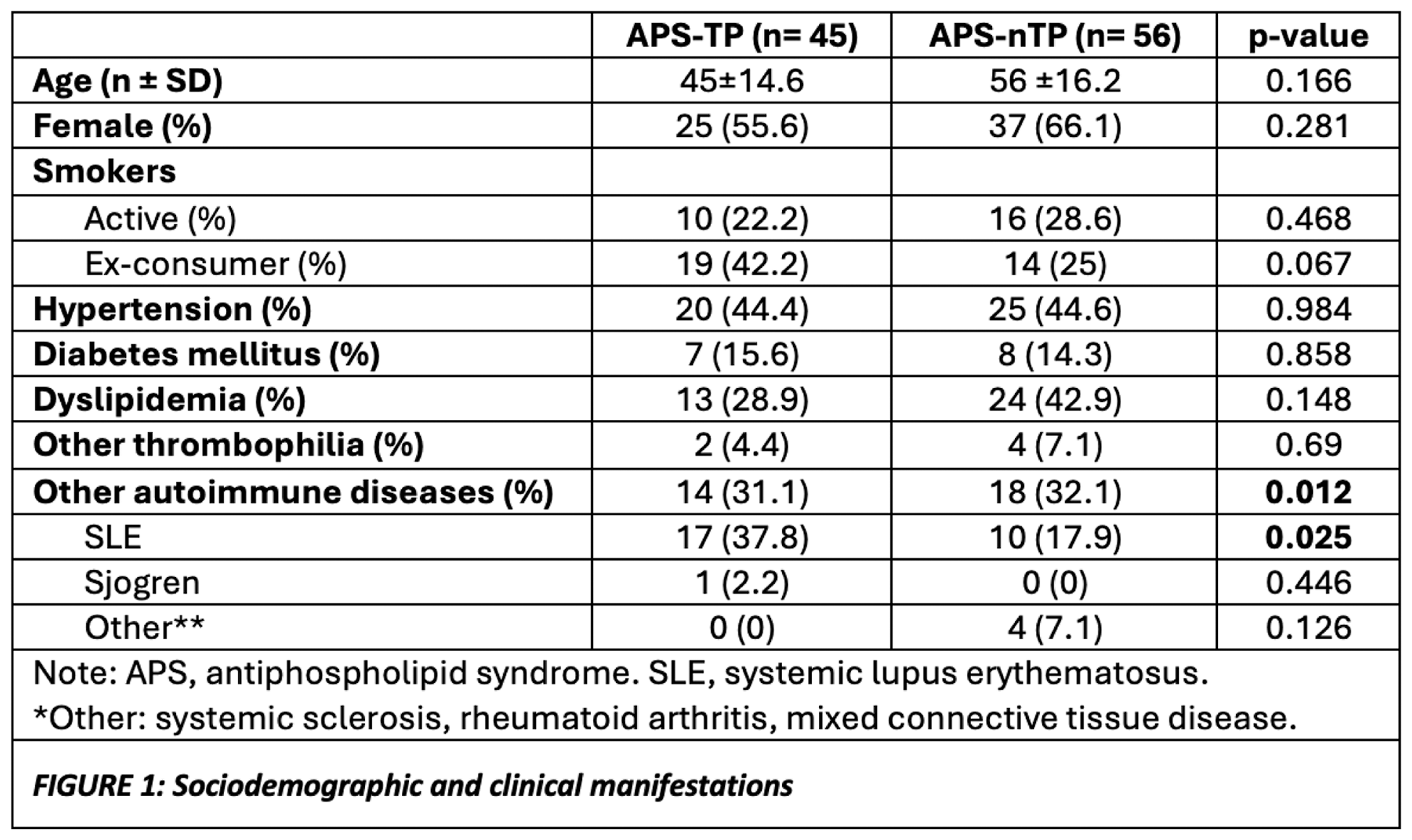
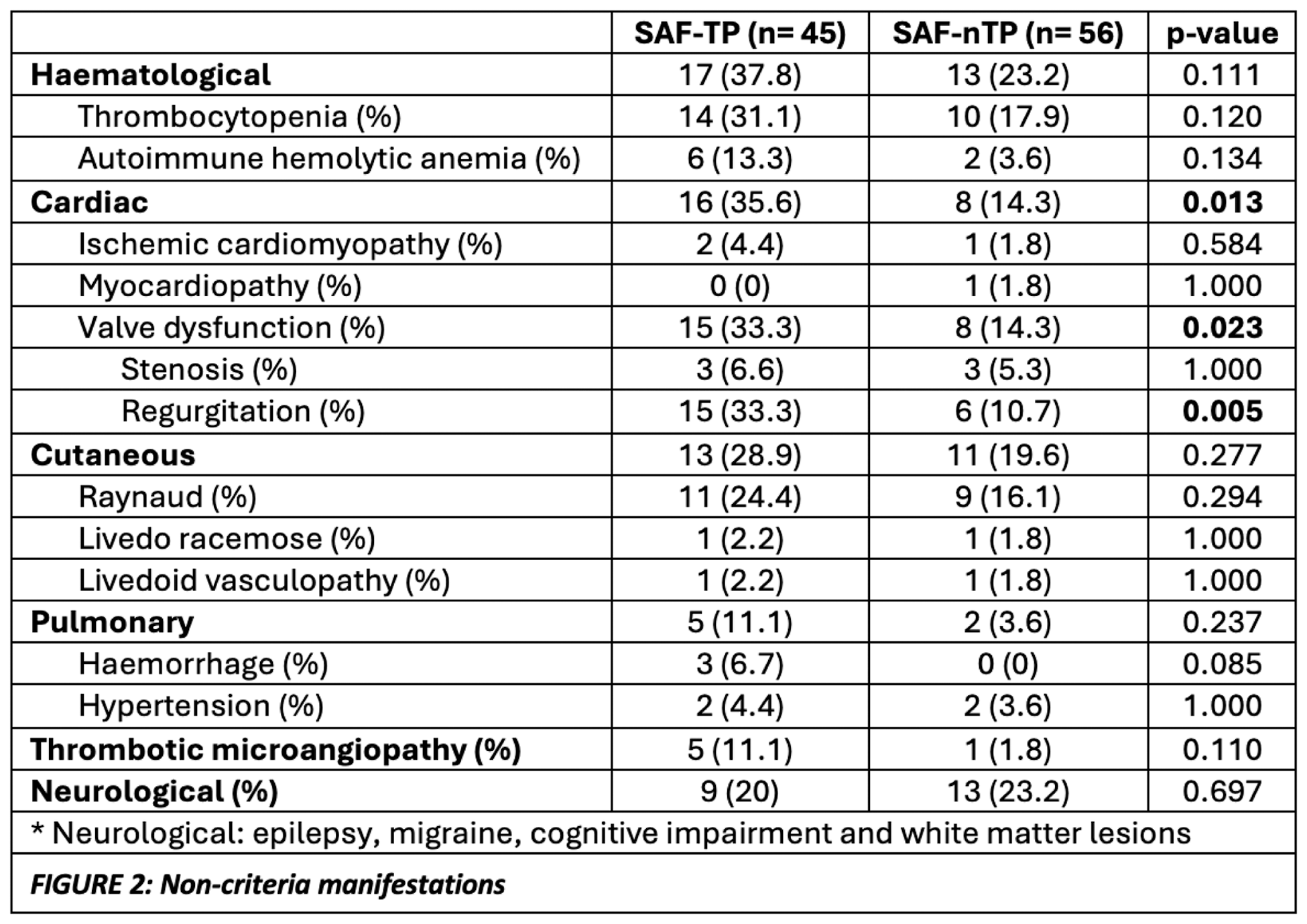
Results: A total of 101 patients were included. The majority of patients were female (n=62, 61.4%), and the mean age was 53 years (Figure 1). Regarding baseline characteristics, Systemic Lupus Erythematosus (SLE) was significantly more frequent in patients APS-TP (p=0.025). Clinically, 22 patients (21.8%) presented obstetric manifestations and 66 (65.3%) thrombotic manifestations (25 [37.9%] arterial, 36 [54.5%] venous and 5 [7.6%] arterial and venous). There were 6 [5.9%] with catastrophic APS. Regarding the non-criteria manifestations, given their wide heterogeneity, they are summarized in Figure 2. When analysing the differences in the presence of non-criteria manifestations between patients with APS-TP and APS-nTP, cardiac manifestations were significantly more frequent in APS-TP patients (p=0.013), particularly valvular disease (Figure 2). We also studied the presence of catastrophic APS in relation to triple positivity, and it was observed that it was more prevalent in patients with APS-TP (n= 5 [11.1%] VS 1 [1.8%]), although without statistical significance. Regarding cardiac manifestations, we focused mainly on valvular heart disease given that other manifestations were found to be infrequent (Figure 2). Of the 101 patients analysed, 23 (22.8%) had valve disease, of which 15 [33.3%] were APS-TP compared to 8 [14.3%] that were APS-nTP (p = 0.023). Valvular regurgitation was more common than stenosis (n= 21 [20.8%] VS 6 [5.9%], respectively) and the mitral valve was the most affected valve in both groups (n= 17 [16.8%]).
Conclusion: In our cohort, patients with APS-TP presented significantly more cardiac manifestations, particularly valvular disease. We did not find differences in the rest of the non-criteria manifestations. No clinical manifestation was found to be more frequent in patients with APS-nTP. In both groups, valve insufficiency was more common than stenosis and the mitral valve was the most affected. Finally, we observed a higher presence of SLE in patients with APS-TP. In this context, a subanalysis of the presence of valvular disease according to TP and co-diagnosis of SLE was performed, and we did not find more presence of valvular disease in patients with APS secondary to SLE.
REFERENCES: NIL.
Acknowledgements: To Ivette and Judit.
Disclosure of Interests: None declared.