

Background: Online symptom checkers (OSCs) could provide guidance in the diagnostic process. The number of OSCs are expanding yet often lack rigorous validation. Rheumatic? is an online questionnaire designed to provide a fast and reliable risk assessment of possible rheumatic diagnoses for individuals with musculoskeletal complaints (MSCs).
We set out to validate this tool by following individuals with MSCs. A key question is representativity of the participants as attrition bias can complicate the construction of a precise prediction model.
Objectives: This project aims to assess aspects of attrition and selection bias in Rheumatic? by comparing participants who did and did not respond to the first follow-up survey, by comparing participants versus patients from general practitioners (GP) and rheumatology clinics, and by exploring variations in characteristics across different recruitment policies.
Methods: Rheumatic? includes a baseline questionnaire about current symptoms and past diagnoses. Participants were recruited online, at primary care or at rheumatology outpatient clinics. Four surveys followed after 0, 3, 6 and 12 months, about source of recruitment, medication, further diagnoses etc. We considered data of July 2021 to July 2023.
We compared participants who solely answered the questionnaire to those who also answered the first follow up survey. Secondly, we compared characteristics of participants across different sources of recruitment (i.e. at primary or secondary care clinics or online (Instagram, Facebook, Google, the Dutch Arthritis Association)). For this, we calculated differences in percentages with confidence intervals and applied chi squared tests.
We assessed representability of the cohort with the expected target population by comparing age, sex and BMI of the participants with information on new patients with MSC from the same period at primary care (GP), Rheumatology clinics in the South West of the Netherlands (RZWN), and the Rheumatology department of Leiden University Medical Centre (LUMC).
Results: A total of 31,457 participants filled out the questionnaire and received an invitation for the first follow up survey. The majority (76 %) was female, 50-60 years old (31 %), and never-smokers (66 %). The number of responses to the follow up survey was (15,591, 50 %) was
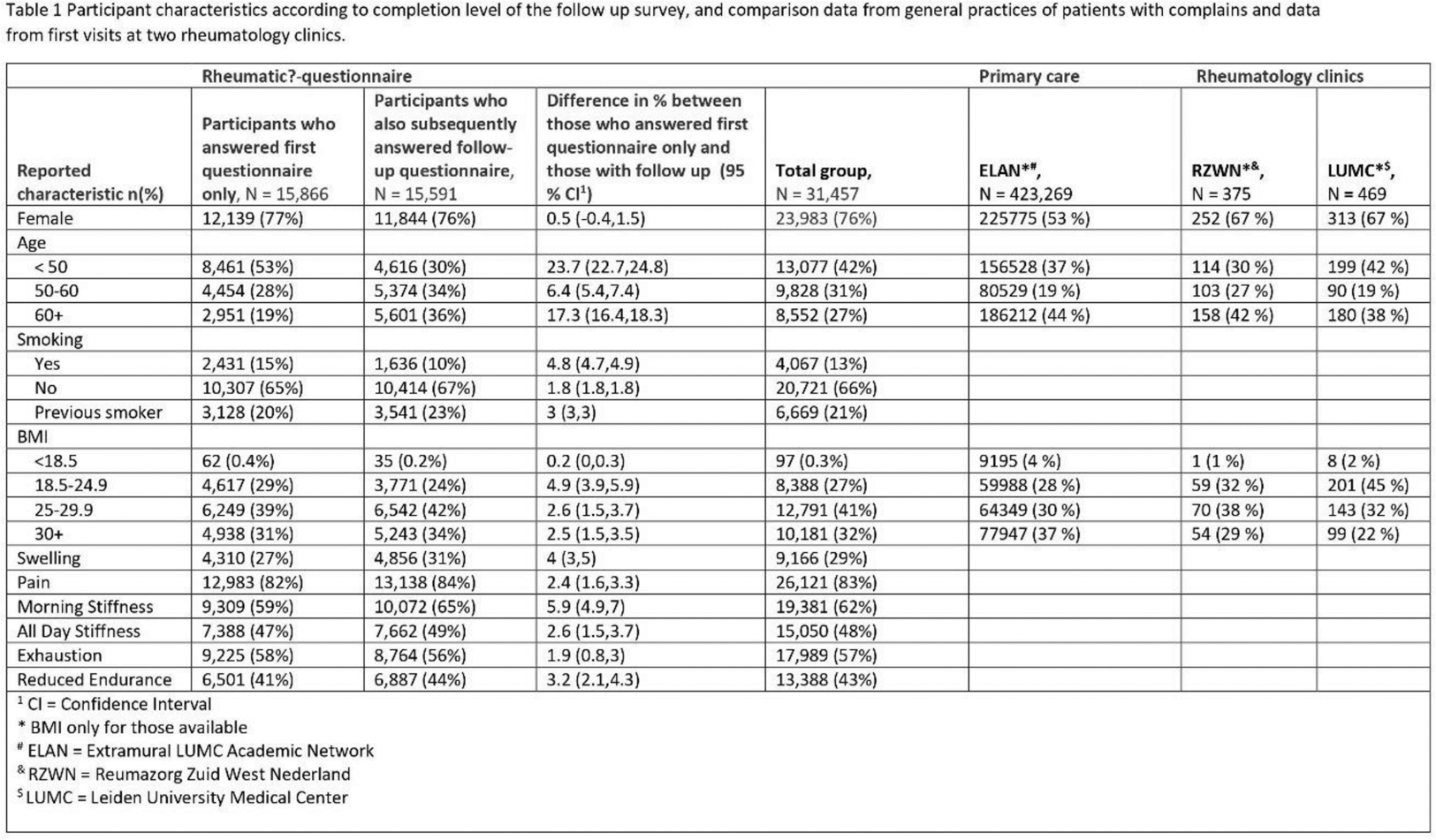
Characteristics like reporting pain, all day stiffness and endurance were similar between those who did and did not answer the follow up survey. We observed higher age, less smoking history and more swelling and morning stiffness for those with follow up (Table 1).
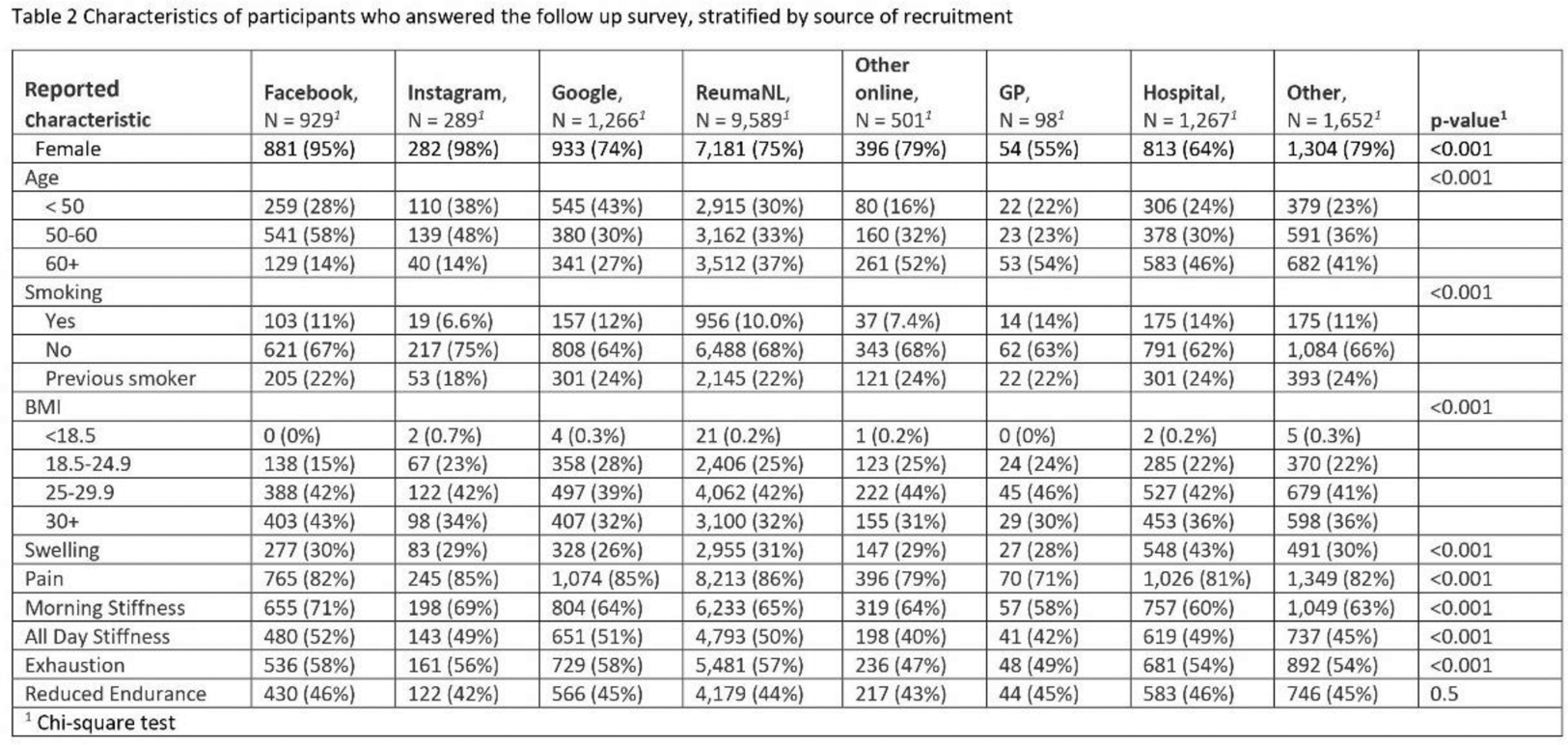
Most participants (12,574, 81 %) found the questionnaire online (mainly via the Dutch Arthritis Associations website (9,589, 62 %)). There were clear differences in characteristics between different sources of recruitment (Table 2). In particular participants recruited by Instagram or Facebook ads were mostly female. The oldest were least often recruited via online sources.
The percentages of females in our cohort was higher than the rheumatology clinics (67 %) and GP (53 %). This higher rate of females was also observed in other studies on OSCs [1,2]. The average age in our cohort was younger. The BMI was comparable to RZWN, but higher than primary care and LUMC.
Conclusion: Our study is one of the first OSCs recruiting real life participants for research. The response rate of the follow up survey was 50 %, comparable to other studies including RA patients recruited via mail (49 %) [3] and general response rates (44 %) [4]. Men were less likely to fill in the OSC, and younger people were less inclined to respond to the follow up survey. Other longitudinal studies similarly found less follow up with younger age [5]. Recruitment via social media may result in overrepresentation of young women. These factors of attrition bias are important to consider when building an accurate symptom checker.
REFERENCES: [1] Pairon A et al, Front Med 2022.
[2] Kopka M et al, J Med Int Res 2023.
[3] Garcia I et al, Arth Care Res 2014.
[4] Wu MJ et al, Comp Hum Behav Rep 2022.
[5] Okpara C et al, Bmj Open 2023.
Acknowledgements: This study was supported by Horizon-EU within the SPIDERR-project (activity No. 101080711), and the DigiPrevent programme (funded in April 2022) from EIT Health. The project has further received funding by the Dutch Organization for Health Research and Development (ZonMw) via the Klinische Fellow No. 40-00703-97-19069, and Open Competitie, No. 09120012110075. A special thank you to David Steeman for data management.
Disclosure of Interests: Floor Zegers: None declared, Ling Qin: None declared, Daniyal Selani: None declared, Georgy Gomon: None declared, Tjardo D. Maarseveen: None declared, Herman Kasper Glas: None declared, Astrid van Tubergen Galapagos, Johnson and Johnson, Novartis and UCB, Yvonne Goekoop-Ruiterman: None declared, Marcel J.T. Reinders: None declared, Erik B. van den Akker: None declared, Corné Baatenburg de Jong: None declared, Lars Klareskog: None declared, Barbara Axnäs ELSA Science, Ewout Steyerberg: None declared, Reinhard Bos Galapagos, Sanofi and consulting fees from Abbvie, Galapagos, Janssen, Pfizer, UCB, Saskia Le Cessie: None declared, Rachel Knevel: None declared.