

Background: Uveitis is the most common extra-articular manifestation of juvenile idiopathic arthritis (JIA), affecting 10-20% of patients. Approximately 88% of patients with JIA-associated uveitis (JIA-U) present within the first 4 years of JIA. Despite adherence with ophthalmic screening examinations based on known clinical risk factors, 50% of children with JIA-U still develop ocular damage. Early detection of JIA-U is crucial for timely treatment to prevent vision-threatening complications.
Objectives: To identify genetic risk factors associated with uveitis in children with JIA.
Methods: We performed a genome wide association study (GWAS) of 144 patients with JIA (88 JIA without uveitis for ≥4 years and 56 JIA-U) of European ancestry from the Predicting Eye Disease in JIA-U (PEDIA-U) study. Ophthalmology examinations confirmed the presence of uveitis. Genotyping was done on the Affymetrix Genome-Wide Human SNP 6.0 array with standard quality control and population substructure, and tested for association via logistic regression adjusting for sex and age of onset of arthritis.
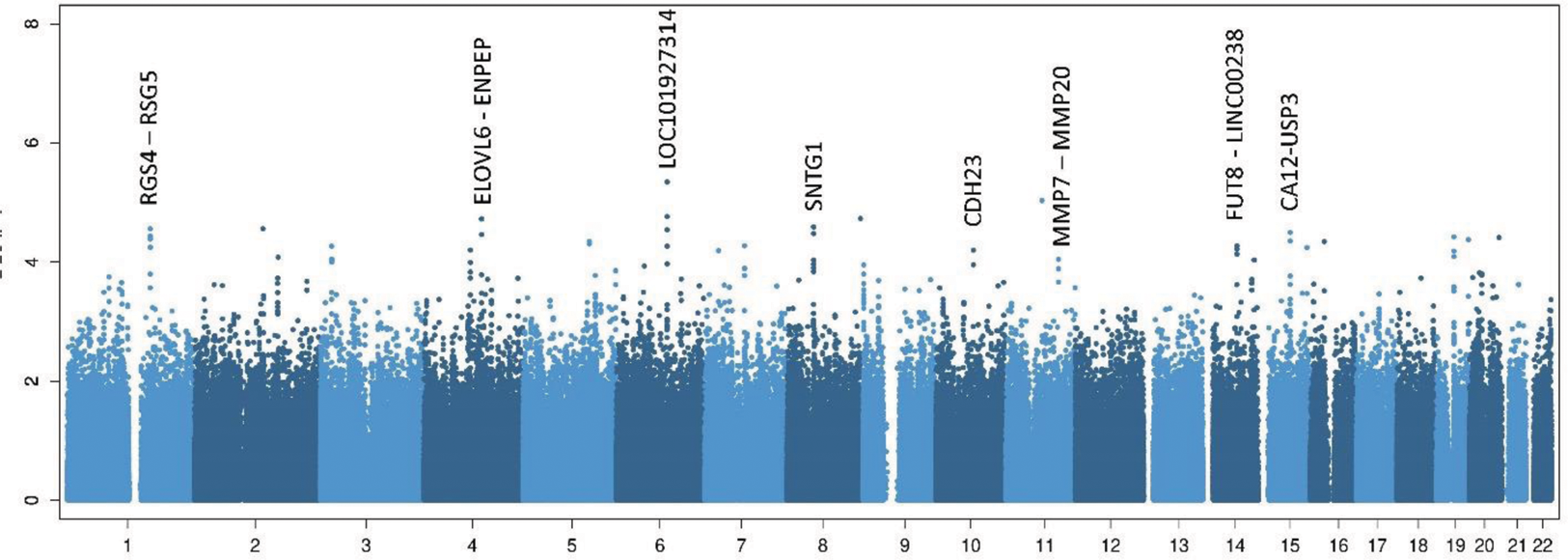
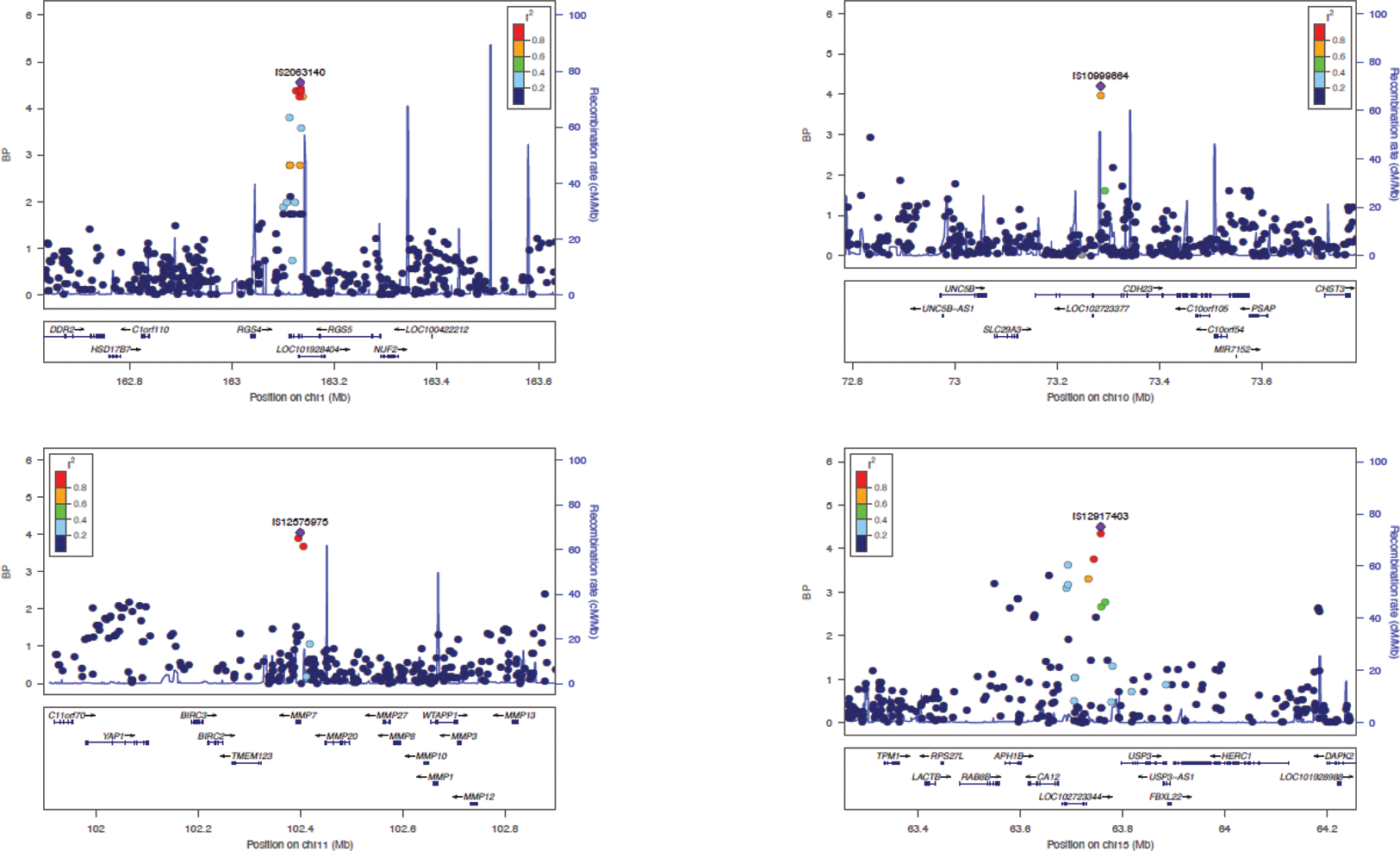
Results: We identified multiple genomic regions with single nucleotide polymorphisms (SNP) associated with uveitis at p<10 -4 (chromosome, SNP, odds ratio, p-value) that have proximal genes linked to ocular disease (Figures 1 and 2). Specifically, 1q23.3 contains rs2063140 (OR=3.7, P=2.75x10 -5 ) which is intronic within RGS4 , a regulator of g-protein signaling 4 and has a role in the development of chronic experimental autoimmune uveitis and neural tissue development. Within 4q25, rs243952 (OR=5.98, P=1.88 ×10 -5 ) is an eQTL for ENPEP and CASP6 . 6q16 contains rs17808421 (OR=4.67; P=4.54 ×10 -6 ) which is near LOC101927314 . On 8q11.21, rs3922033 (OR=0.17, P=2.57 ×10 −5 ) is located within SNTG1. On 10q22.1, rs10999864 (OR=7.24, P = 6.31 ×10 −5 ) is within CDH23 , a gene implicated in Usher syndrome. On 11q22.2, rs12575975 (OR=4.95, P = 8.98 ×10 −5 ) is located within MMP7 and is an eQTL for MMP7. Matrix metalloproteinases such as MMP7 are upregulated in a rat model of experimental autoimmune uveoretinitis, increase the permeability of the blood-brain barrier in an experimental autoimmune encephalomyelitis, and implicated in neovascular complications of age-related macular degeneration in humans. 14q23.3 (rs12589911, OR=10.11 P=5.36 ×10 -5 ) is located near FUT8 - LINC00238 . On 15q22, rs12917403 (OR=5.91, P = 3.17 ×10 −5 ) is an eQTL in various tissues for multiple genes, including CA12 , LINC02568 , HERC1 , and RPS27L. CA12 is a carbonic anhydrase and zinc metalloenzyme that contributes to formation of aqueous humor and RPS27L is linked to retinitis pigmentosa 23.
Conclusion: Even with this small GWAS, multiple genomic regions are associated with JIA-U compared to JIA without Uveitis, including regions with genes related to ocular function and disease. Expansion of the deeply phenotyped cohort is underway for validation and more power tests of associations. Identifying genetic polymorphisms may help identify important JIA-U pathways and pharmacologic targets. It will also lead to the development of genetic risk scores for JIA-U.
Manhattan plots highlighting 8 JIA-U associated regions
LocusZoom plots for 4 key associated regions
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.