

Background: Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in children. Numerous studies have indicated that 20-40% of JIA patients undergoing various biological treatments face the challenge of joint relapse. However, there is a lack of information regarding risk factors for disease flare-ups under biological treatment [1-5].
Objectives: This study aims to assess the incidence of disease flare-ups in patients receiving biological treatment and to identify the risk factors contributing to such flares in comparison to those who remain flare-free.
Methods: A multicenter retrospective follow-up study was conducted on children aged 0-18 years from three tertiary centers in Israel, with polyartricular disease, diagnosed with one of the relevant subtypes of JIA and treated with any form of biological therapy. Demographic and clinical data were collected. Patients were divided into groups based on the presence or absence of joint flare-ups. The groups were compared to identify risk factors. In addition, survival analysis was conducted for the 2 groups.
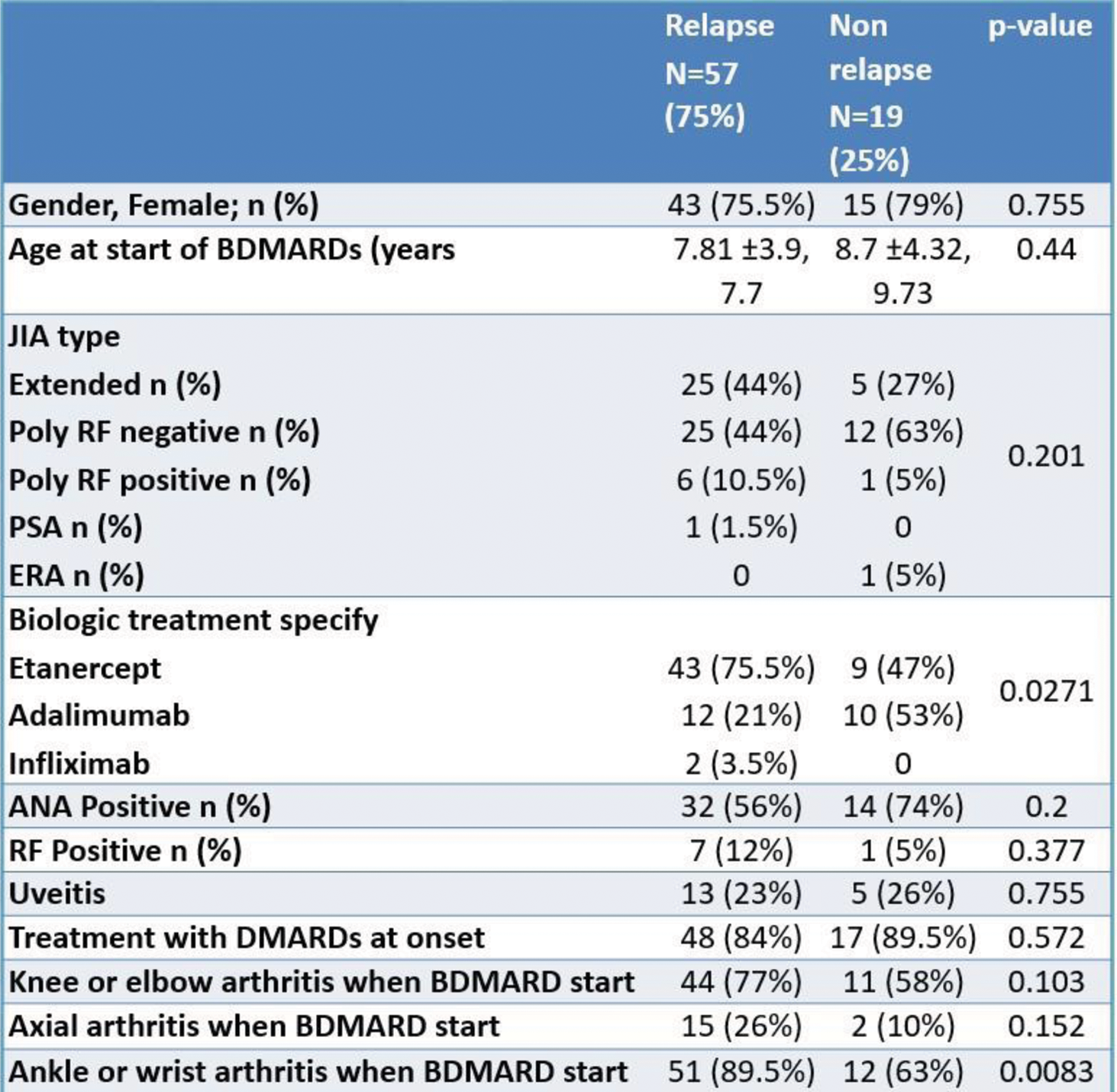
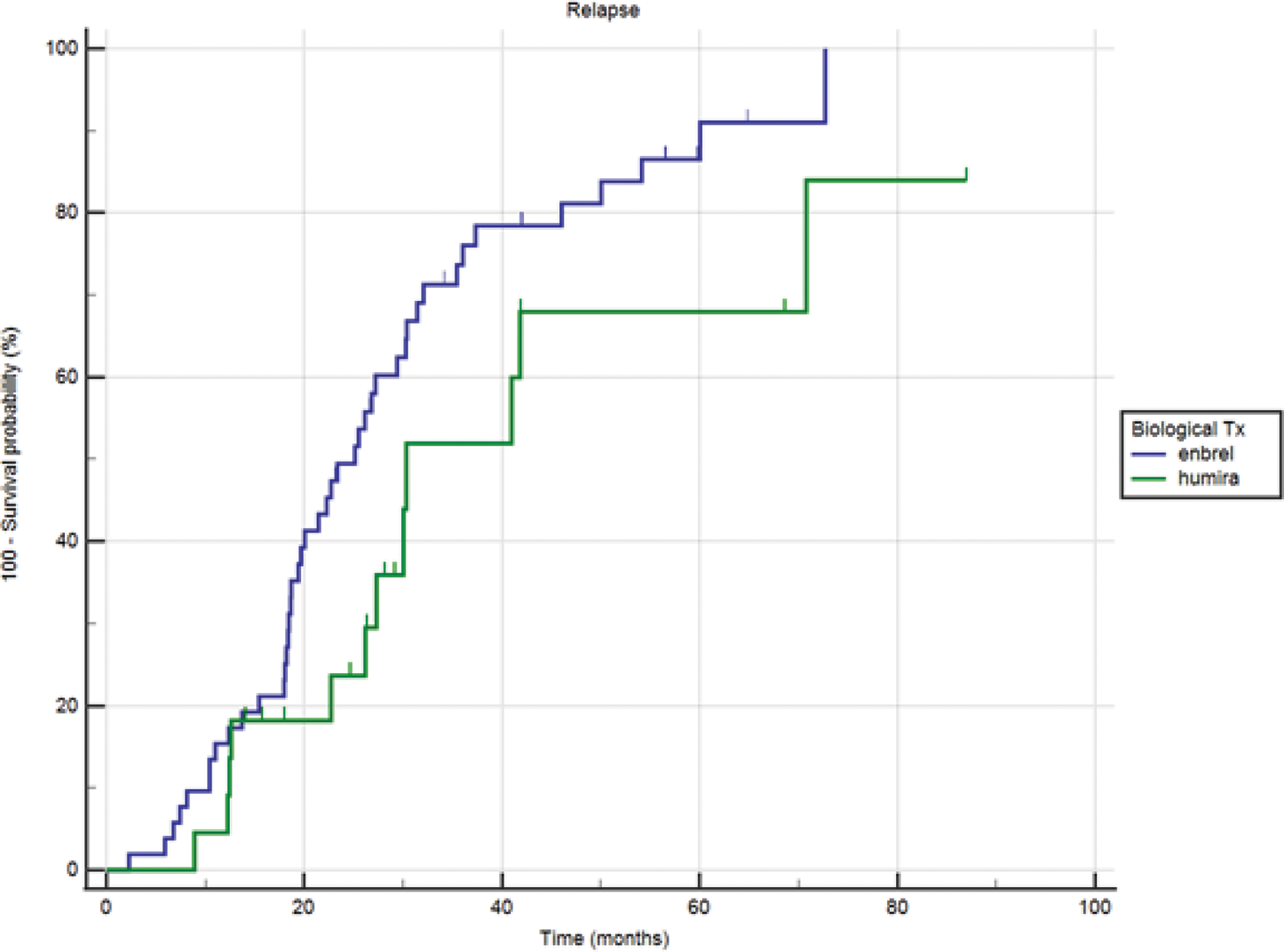
Results: Seventy-six children met the inclusion criteria. The median age of disease onset was 4.65 years (range: 2.1-9.49 years), and the median age of achieving CID was 8.5 years (range: 5.7-11.85 years). Seventy-five percent of the children experienced flare-ups under biological treatment, with a median time from CID to flare-up of 1.2 years (range: 0.68-1.89 years). Children treated with Etanercept as the first biological therapy had four times more relapse events compared to those treated with Adalimumab (OR = 3.98, 95% CI: 1.31-12.01, p-value = 0.0142). Involvement of the wrist or ankle joint at the start of biological treatment was significantly associated with flare-ups compared to patients without involvement of these joints at treatment initiation (OR = 4.76, 95% CI: 1.35-16.79, p-value < 0.0152).
Conclusion: JIA patients with multiple joint involvement who initiated biological treatment are at a high risk of experiencing flare-ups (75%). Risk factors for relapse include wrist or ankle involvement at presentation and initial treatment with Etanercept compared to Adalimumab.
REFERENCES: [1] Macaubas C, Nguyen K, Milojevic D, Park JL, Mellins ED. Oligoarticular and polyarticular JIA: epidemiology and pathogenesis. Nat Rev Rheumatol. 2009 Nov;5(11):616-26.
[2] Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135.
[3] Iglesias E, Torrente-Segarra V, Bou R, Ricart S, González MI, Sánchez J, Calzada J, Antón J. Non-systemic juvenile idiopathic arthritis outcome after reaching clinical remission with anti-TNF-α therapy: a clinical practice observational study of patients who discontinued treatment. Rheumatol Int. 2014 Aug;34(8):1053-7.
[4] Gieling J, van den Bemt B, Hoppenreijs E, Schatorjé E. Discontinuation of biologic DMARDs in non-systemic JIA patients: a scoping review of relapse rates and associated factors. Pediatr Rheumatol Online J. 2022 Dec 5;20(1):109.
[5] Castillo-Vilella M, Giménez N, Tandaipan JL, Quintana S, Modesto C. Clinical remission and subsequent relapse in patients with juvenile idiopathic arthritis: predictive factors according to therapeutic approach. Pediatr Rheumatol Online J. 2021 Aug 21;19(1):130.
Table 1.
Acknowledgements: NIL.
Disclosure of Interests: None declared.