

Background: Microvascular changes represent a key step of pathogenic process in Systemic Sclerosis (SSc). However, macrovascular complications have also been reported, especially configuring lower extremities arterial disease (LEAD). Possible risk factors were identified as digital ulcers (DU), pulmonary arterial hypertension (PAH), corticosteroids and smoking (active/stopped <3 years) 1 .
Objectives: Our aim was the estimation of LEAD prevalence in: (i) a single-centre prevalent SSc cohort; (ii) at-risk SSc patients according to the above-mentioned parameters 1 .
Methods: Consecutive SSc patients (ACR/EULAR 2016 classification criteria) attending our Centre for scheduled visits (October 2022-December 2023) were included. Patients without known LEAD presenting ≥1 risk factor, as described above, were referred for lower extremities arterial Doppler ultrasonography (DUS) performed by a single expert vascular surgeon. LEAD was classified according to Leriche-Fontaine stages: asymptomatic (stage I), claudication (stage II), ischemic rest pain (stage III) and ulceration/gangrene (stage IV).
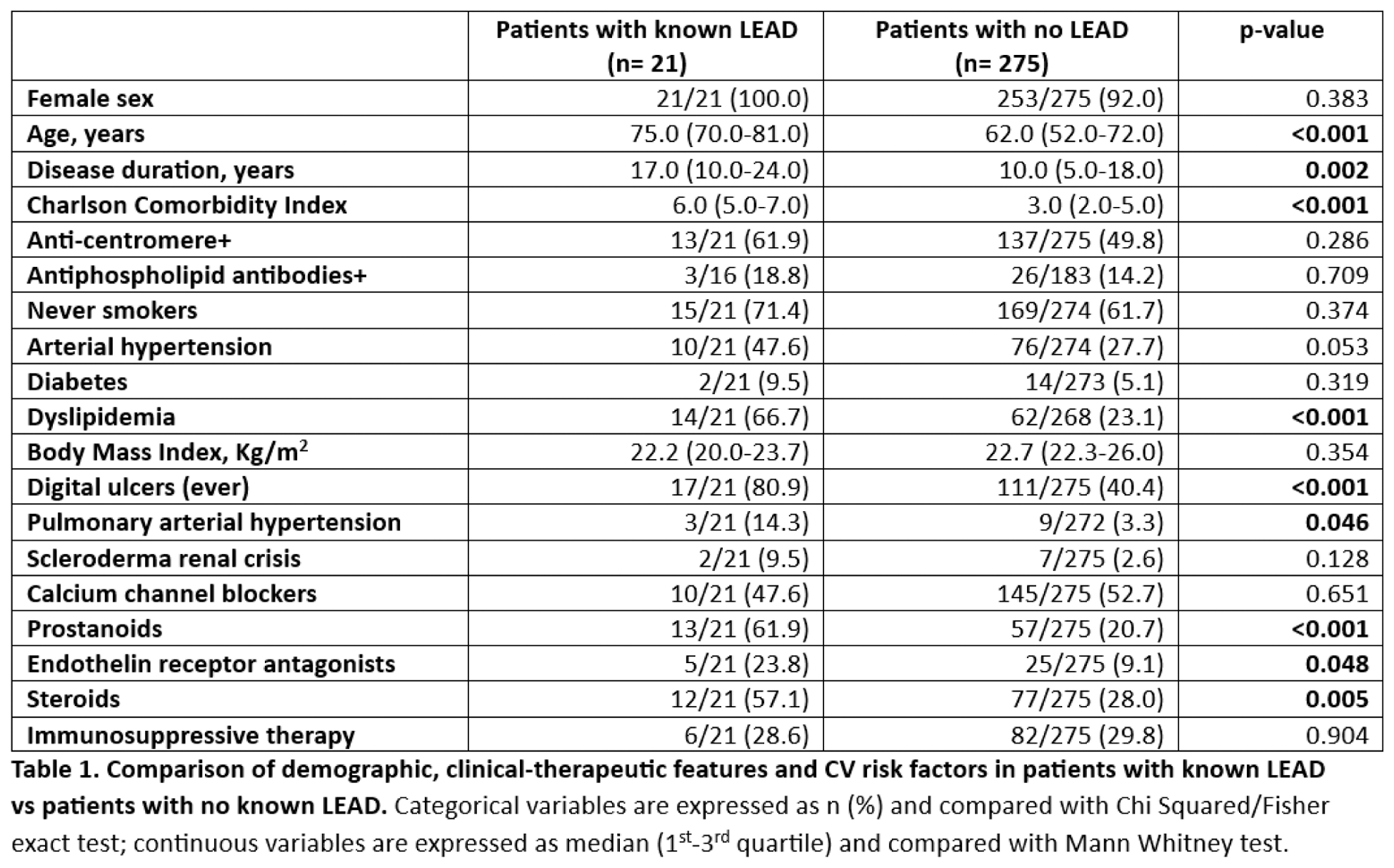
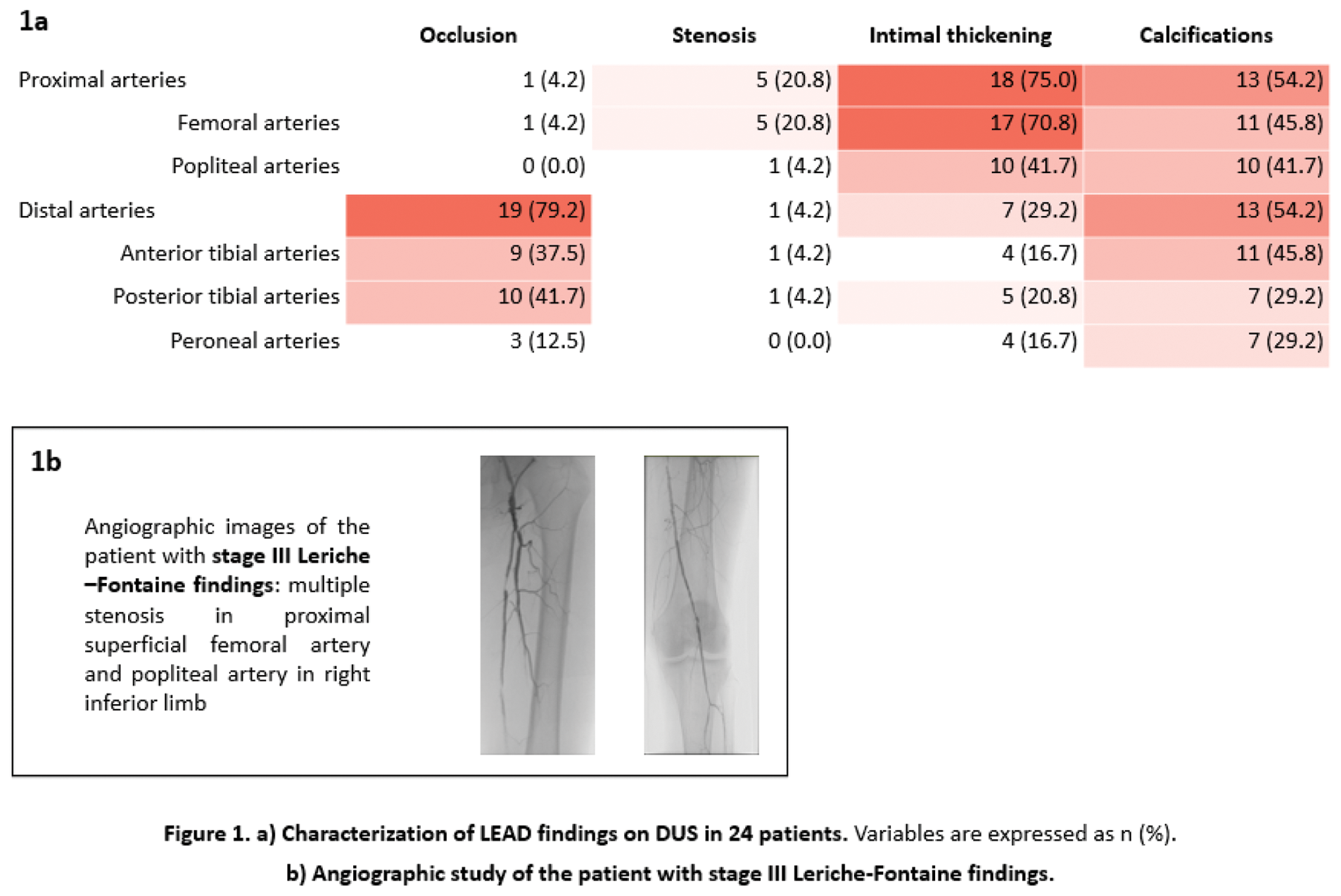
Results: Among 296 SSc patients evaluated (93% females, 85% limited cutaneous involvement, 51% anti-centromere+) in the indicated period, 21 (7%) were previously diagnosed with LEAD, requiring revascularization interventions in 9 (43%) and amputations in 5 (24%). As compared to the remaining 275, the formers were older, had longer disease duration, higher frequency of vascular complications, presented more comorbidities and were more frequently treated with vasodilators and steroids ( Table 1 ). At least 1 LEAD risk factor was identified in 176/275 (64%) patients without known LEAD (DU (59%); steroid use (44%); smoking (27%); PAH (5%)). Among them, 75/176 received DUS, with detection of LEAD in 24 (32%) ( Figure 1a ), classified as 20 stage I, 3 stage II (without disabling claudicatio) and 1 stage III. Anti-platelet/anti-coagulant therapy was already ongoing in 17/24, while in the remaining 7 low dose aspirin was added. The patient with stage III was referred to angiographic study and underwent percutaneous transluminal angioplasty ( Figure 1b ). As compared to 51 at-risk patients without LEAD, they were older (70.0 [61.8-73.5] vs 60.0 [54.5-70.5] years, p: 0.061), more frequently active smokers (50.0% vs 23.5%, p: 0.022), exhibited more frequently telangiectasias (91.7% vs 62.0%, p: 0.008) and were less commonly treated with vasodilators (75.0% vs 94.1%, p: 0.026).
Conclusion: Based on this preliminary data, the prevalence of diagnosed LEAD in our SSc cohort is 7%. However, screening of at-risk patients (DUs, PAH, steroid use and smoking), showed DUS LEAD signs in up to one third of the patients, mostly asymptomatic, who deserve regular follow-up and possibly correction of modifiable risk factors. Therefore, lower extremities arterial DUS is a non-invasive helpful tool to improve SSc diagnostic/therapeutic work-up, in which vascular surgeon should become active part of the dedicated multidisciplinary team.
REFERENCES: [1] Bertolino et al. JSRD. 2020.
Acknowledgements: The Authors would like to thank GILS “Gruppo Italiano Lotta Sclerodermia” for substantially supporting the study with a grant
Disclosure of Interests: None declared.