

Background: Systemic sclerosis (SSc) is a disease with a high morbidity and mortality. As other autoimmune systemic diseases, it is associated with early atherosclerosis and increased cardiovascular risk. Nailfold capillaroscopy is a widely use method for the diagnosis and monitoring of SSc.
Objectives: To describe the frequency of subclinical vascular damage, major adverse cardiovascular events (MACEs) and mortality in a cohort of patients with SSc. To analyse the association and predictive value of nailfold capillaroscopy at the time of diagnosis, with subclinical vascular damage, MACEs and deaths.
Methods: Retrospective observational study. All patients from a longitudinal SSc cohort followed at a hospital in eastern Spain between 1984 and 2023 were included. The demographic data (sex, age, weight, height and body mass index [BMI]), clinical variables (smoking habits, arterial hypertension [PAH], dyslipidemia [DLP], diabetes mellitus [DM], diffuse interstitial lung disease [DIL], pulmonary hypertension [PH], digital ulcers [DUs], modified Rodnan scale score at the time of diagnoses [mRSS] and subtype of SSc) and laboratory data (C-reactive protein [CRP] and erythrocyte sedimentation rate [ESR]) was recorded. Moreover, a qualitative analysis of the findings in the nailfold capillaroscopy at the time of the diagnosis was made. Subclinical vascular damage (aterosclerosis) was evaluated by extracranial carotid artery ultrasound (ESAOTE MyLab XV70) or examining patients’ CT scans. MACEs and deaths, as well as their respective causes, were obtained from the patient’s medical history. A regression model was created, examining the effect of the findings in the nailfold capillaroscopy on the clinical events.
Results: A total of 175 patients, 93% women, were included. 80% were classified as limited SSc and 20% as diffuse SSc, with a mean age of 53 years (SD ± 16.07). The mean weight was 65.01kg (SD ± 12.85), the mean height was 1.59m (SD ± 0.08) and the mean BMI was 25.56kg/m 2 (SD ± 4.81).
Of our sample, 15.4% were active smokers and 22.29% had a previous history of smoking. 35% had DLP, 33% PAH and 7% DM. At the time of the diagnosis, the mean CRP was 8.05mg/L (SD ± 16.21) and the ESR was 12.64mm/h (DE ± 13.16). During the follow-up period, 27.23% developed UDs, 26.29% were diagnosed of ILD and 13.14% of PH.
In the nailfold capillaroscopy at baseline, 85.71% presented with scleroderma patterns of microvascular damage. From these, 84% exibited megacapillaries, 72.67% hemorrhages and 57.33% avascular areas.
Of our cohort, 49% had subclinical macrovascular damage in the form of atherosclerosis. After a mean follow-up of 10 years (SD ± 7.84), 19% of patients suffered at least one MACE (50% heart, 32% peripheral and 29% cerebral) and 22% died. From our total fatalities; 29% of them were attributed to SSc, whereas 37% where secondary to a MACE.
The presence of avascular areas in the baseline nailfold capillaroscopy was found to be related to PAH (p = 0.008), PH (p = 0.001), DUs (p = 0.0019), modified Rodnan scale score at baseline (p = 0.000), MACEs (p = 0.008), cerebral vascular event (p = 0.0018), total number of MACEs (p = 0.008) and death by any cause (p = 0.000). We found no statistically significant associations between megacapillaries and hemorrhages with the studied variables.
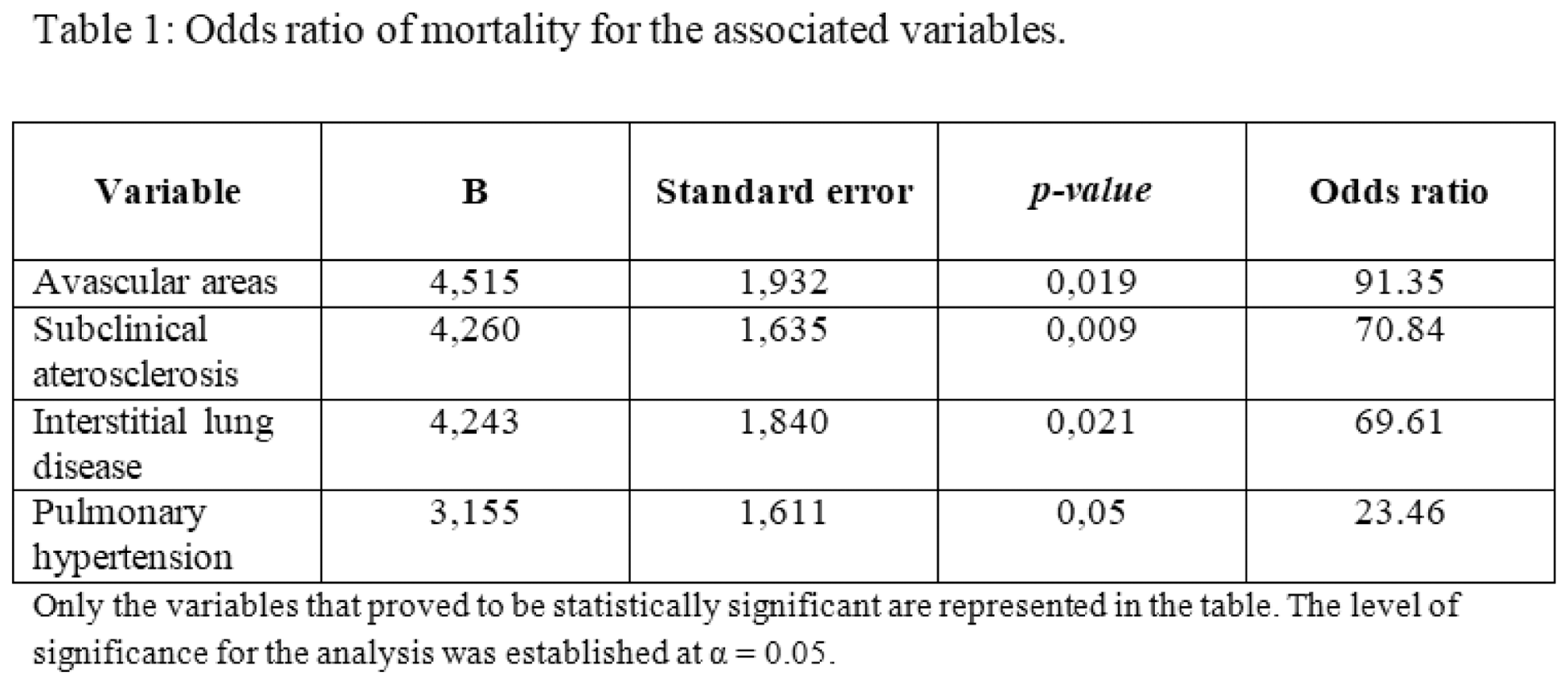
A regression model was created to analyse the effect of the studied variables with MACEs and mortality. The estimated Odds ratio (OR) of fatality was 91.35 times higher in patients with avascular areas in their baseline nailfold capillaroscopy. This OR was even higher than that of subclinical atherosclerosis (70.84), ILD (69.61) and PH (23.46), as summarised in Table 1.
Conclusion: Patients with SSc have an increased risk of atherosclerosis, MACEs and death. The presence of avascular areas in nailfold capillaroscopy at baseline was a risk factor for mortality in our cohort.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.