

Background: Counseling plays a fundamental role in women affected by rheumatic diseases (RMDs) to ensure the best possible outcomes and should be started as early as possible.
Objectives: The study aims to give an overview about the management of family counseling in women affected by RMDs in Italy
Methods: Nineteen Italian centers were involved. Women of childbearing age (18 to 50 years) affected by RMDs were included. Data about diagnosis, disease activity, treatment were collected during routine visits. Information about family planning was obtained through a survey including 19 questions. Data were collected from December 2021 to March 2022 and from October to December 2022.
Answers from questionnaires collected from women were expressed by absolute numbers and percentage for categorical variables and mean ± deviation standard for continuous variables.
To compare the groups in case of categorical variables the Chi square test was used or the Exact Fisher test when there was a limited amount of data. For continuous variables, the Student’s T test was used.
Statistical significance was defined as a p value < 0.05.
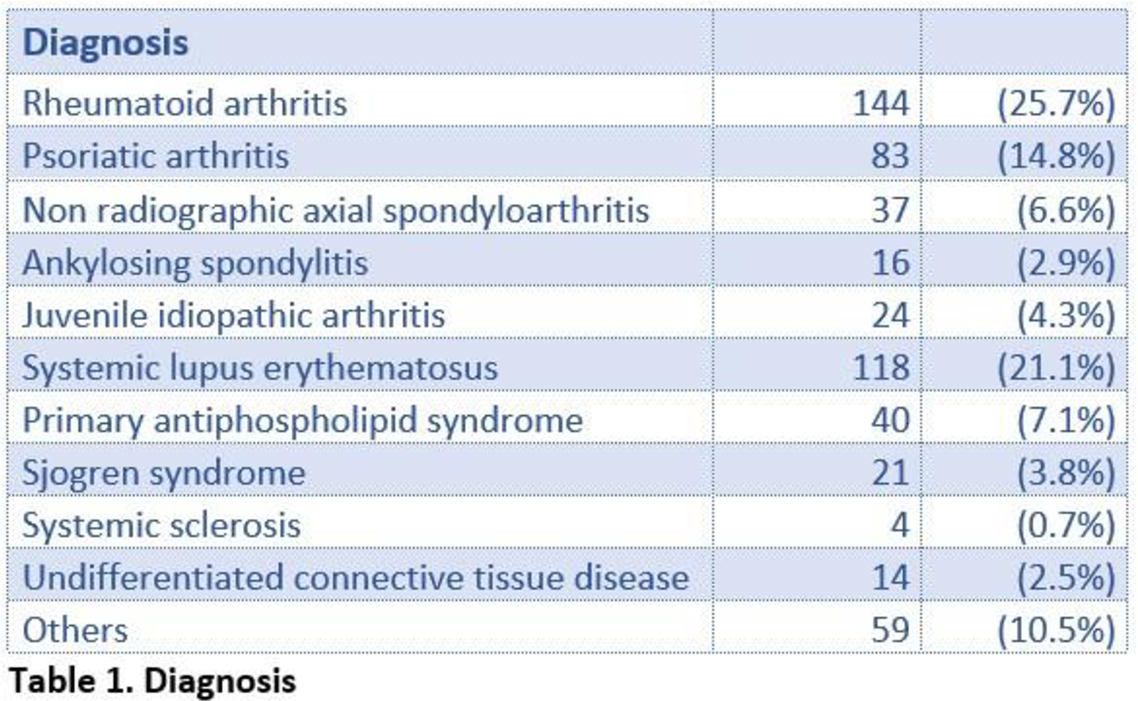
Results: We collected data on 560 patients, mean age 34.2 ± 5.9 years, with a mean disease duration of 8.8 ± 7.6 years. Diagnoses are summarized in Table 1.
Three hundred and fifty-four patients (63%) were at their first counseling, while 112 (20%) were already receiving regular counseling. In 22.7% of cases examination was conducted with another specialist, mostly represented by the gynecologist (89.8%).
Fifty percent of patients were treated with conventional synthetic disease modifying antirheumatic drugs (DMARDs), with hydroxychloroquine being the most frequently used (30%), while a smaller percentage of patients received biologic DMARDs (39.6%), mostly represented by TNF inhibitors (29.6%). Only 1.8% of patients were treated with JAK inhibitors.
At the time of assessment, 135 of patients were planning a pregnancy, 162 were pregnant and 246 were actively avoiding pregnancy. Two hundred-forty-one patients (43%) reported to use a contraceptive method: barrier method in 69%, estroprogestinic in 18% and intra-uterine device in 2.5%; 319 (57%) were not using any contraception. Within this group, 17% were taking medications incompatible with pregnancy.
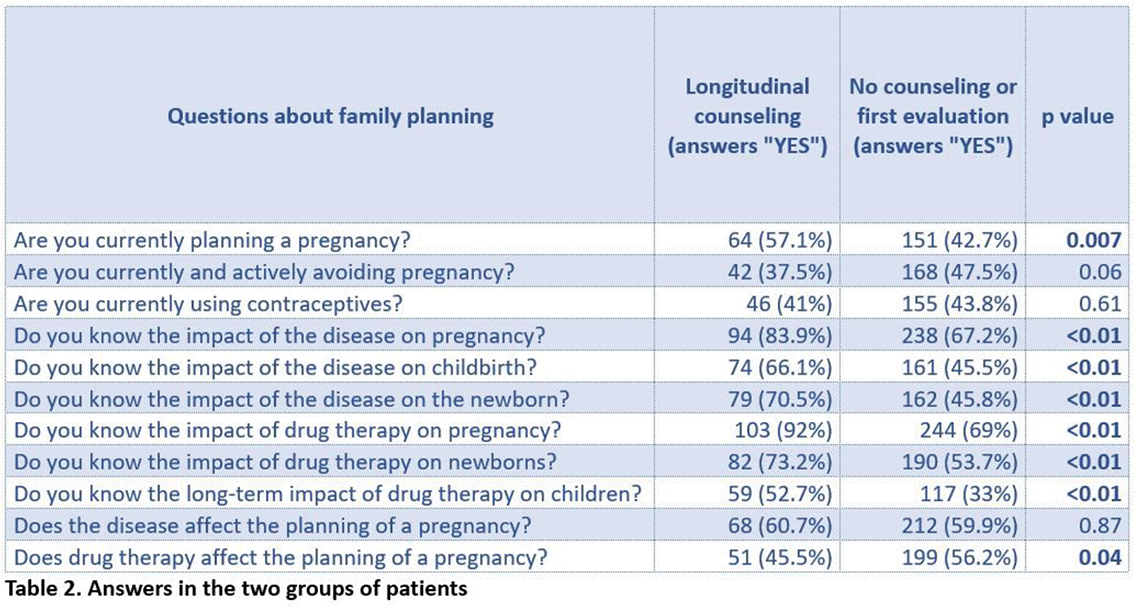
Most patients (72%) were aware of the effects of their disease on pregnancy but only 53% knew about disease impact on the newborn; 74% of patients showed knowledge about the effect of drugs on pregnancy, 59% were aware of the effects of medications on newborns and 40% understood the long-term effects of therapy on their children.
Patients who repeatedly underwent counseling over time had a significantly higher awareness of the disease impact on pregnancy and newborns and of the effects of drug therapy on themselves and their infants in both the short and long term. Answers in the two groups are shown in Table 2.
Conclusion: This study demonstrates that a high percentage of patients knows the impact of RMD on pregnancy and vice-versa but a lack of knowledge about the effects of therapies on the newborn has emerged and need to be improved. It also demonstrates the importance to repeat counseling over time to improve patients’ empowerment. An effort should be made in informing patients about the risk of the lack of contraception or the use of less effective method of contraception, especially in those undergoing treatment incompatible with pregnancy.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Giulia Carrea: None declared, Maria Gerosa UCB, Astrazeneca, Marta Mosca UCB (Advisor), Melissa Padovan: None declared, Sabrina Paolino: None declared, Maria Grazia Anelli: None declared, Roberta Ramonda: None declared, Cecilia Nalli: None declared, Patrizia Rovere-Querini: None declared, Elisa Bellis: None declared, Salvatore D’Angelo: None declared, Enrico Fusaro: None declared, Maria Sole Chimenti Maria Sole Chimenti has received speaker honoraria and/or unrestrictive research grants from Ely, Lilly, Abbvie, Pfizer, UCB, Novartis, Janssen, Leonardo Santo: None declared, Marco Gabini: None declared, Giulia Pazzola: None declared, Francesca Serale: None declared, Carlomaurizio Montecucco: None declared, Fabrizio Conti: None declared, Roberto F. Caporali: None declared.