

Background: Patients with rheumatic and musculoskeletal disease have a high prevalence of chronic kidney disease (CKD), which is associated with increased morbidity and mortality. Despite its high burden, effective treatments for this serious organ involvement are lacking. Sodium-glucose cotransporter 2 (SGLT-2) inhibitors are a new class of oral hypoglycemic agents that improve glycemic control and reduce the risk of cardiovascular events in patients with type 2 diabetes mellitus [1]. However, previous clinical trials excluded patients with rheumatic and musculoskeletal diseases, therefore, little is known about the efficacy and safety of the drug for CKD in patients with rheumatic and musculoskeletal diseases.
Objectives: To elucidate the effectiveness and safety of dapagliflozin, an SGLT-2 inhibitor, in patients with rheumatic and musculoskeletal diseases complicated with CKD and identify factors associated with the response to dapagliflozin.
Methods: We reviewed consecutive patients with rheumatic and musculoskeletal disease and CKD who were treated with dapagliflozin for more than one year. The good response was defined as an improvement in the estimated glomerular filtration rate (eGFR) slope per year after dapagliflozin initiation compared to that before treatment. We investigated the response rate and its predictive factors.
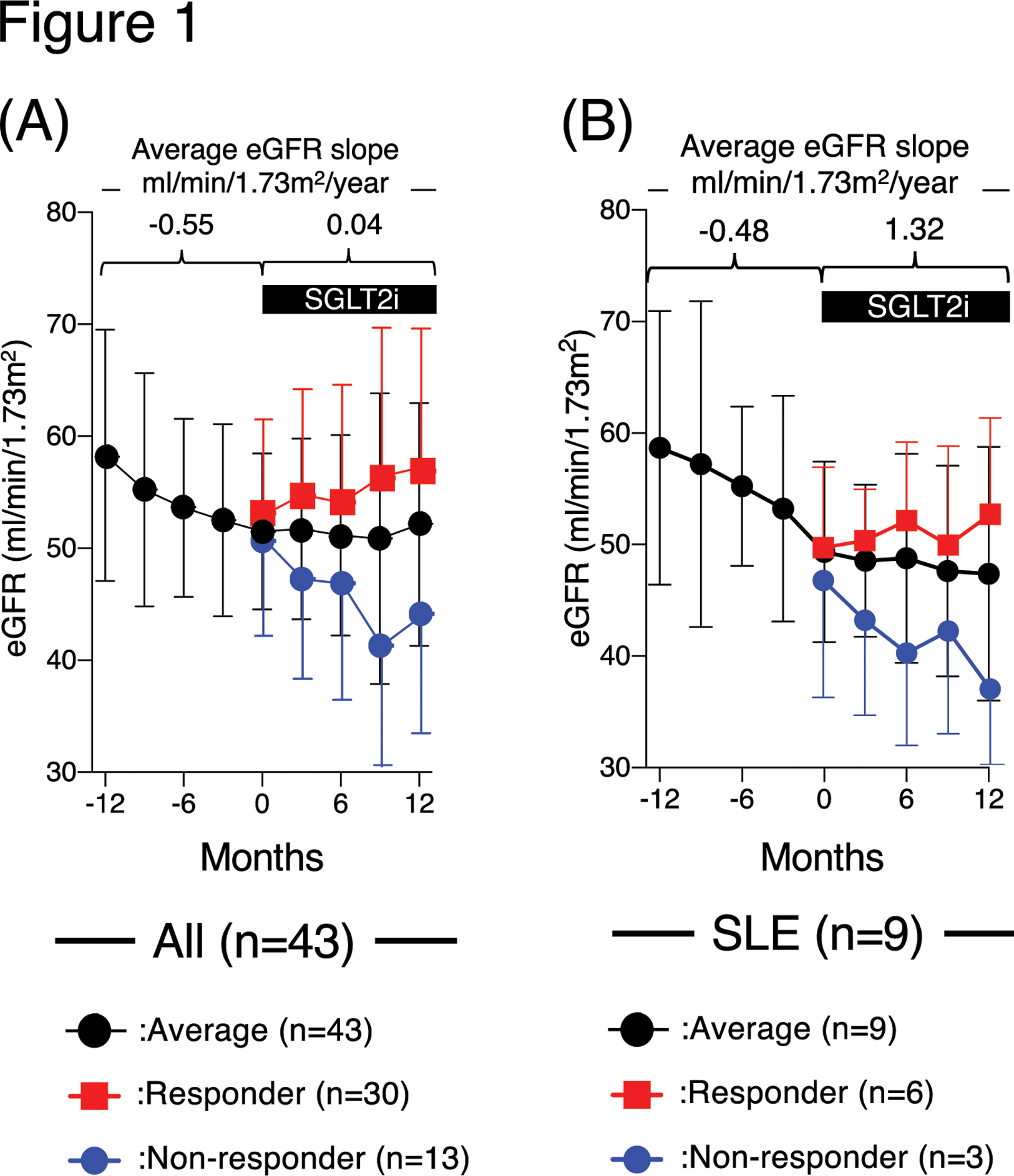
Results: Forty-three patients were included in the analysis. The mean eGFR slope improved significantly after dapagliflozin initiation compared to before the treatment (0.04 ± 0.61 vs -0.55 ± 0.65 mL/min/1.73m 2 /year, p=0.001, Figure 1A), with a good response rate of 69.8%. Especially in SLE patients, improvement of eGFR slope was prominent compared to the other diseases (1.32 ± 0.76 vs 0.04 ± 0.61 mL/min/1.73m 2 /year, p=0.031; Figure 1B). Patients in the good response group showed low levels of C-reactive protein (0.08 ± 0.18 vs 0.25 ± 0.29 mg/dL, p=0.03), used angiotensin II receptor blockers more frequently (80.0% vs 38.4%, p=0.01), and used tacrolimus use less frequently (10.0% vs 76.9%, p<0.01) than those in the non-response group. No serious safety events, including urinary tract infections, hypoglycemia, or dehydration, occurred during dapagliflozin treatment.
Conclusion: Dapagliflozin is effective for rheumatic and musculoskeletal diseases patients with CKD for preventing deterioration of renal function. Antihypertensive treatment with ARBs and inflammation control without tacrolimus use could increase the likelihood of favorable response to dapagliflozin.
REFERENCES: [1] Hanaoka H, Kikuchi J, Hiramoto K, Saito S, Kondo Y, Kaneko Y. Decreased chronic kidney disease in rheumatoid arthritis in the era of biological disease-modifying anti-rheumatic drugs. Clin Kidney J 2022; 15:1373-1378.
Acknowledgements: NIL.
Disclosure of Interests: None declared.