

Background: Modulation of CTLA-4 pathway has been of interest in autoimmune disease and malignancy, although the direction of stimulation is opposed in these two conditions. This raises the question of whether abatacept use (CTLA-4 agonist) could have a detrimental effect on malignancy risk [1]. A recent comprehensive safety analysis highlighted an increased risk of non-melanoma skin cancer (NMSC) with abatacept, compared with conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs)[2]. Whether this risk extends to all malignancies excluding NMSC remains unclear.
Objectives: To estimate the association of abatacept with the incidence of malignancy excluding NMSC, compared with placebo, other biological disease modifying anti-rheumatic drugs (bDMARDs), and conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs) in both randomised controlled trial and real-world settings.
Methods: Systematic searches of databases were performed, to November 2023, to identify phase II/III/IV randomised clinical trials (RCTs) and long-term extension (LTE) studies of abatacept compared with placebo, as well as observational studies comparing abatacept with other bDMARDs and csDMARDs in adults with RA and PsA. Incidence rates (IR) were calculated per 1000 person years. Random-effects meta-analysis was performed to estimate incidence rate ratios (IRRs) for all malignancies, excluding NMSC, between abatacept and comparators in adults with RA or PsA.
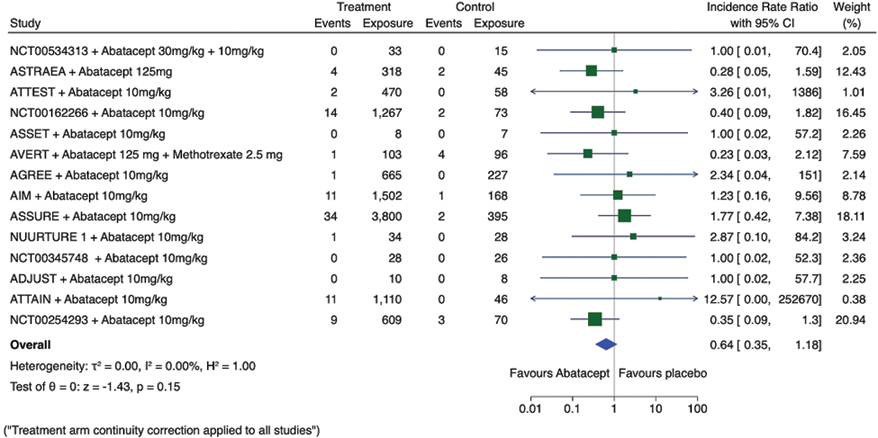
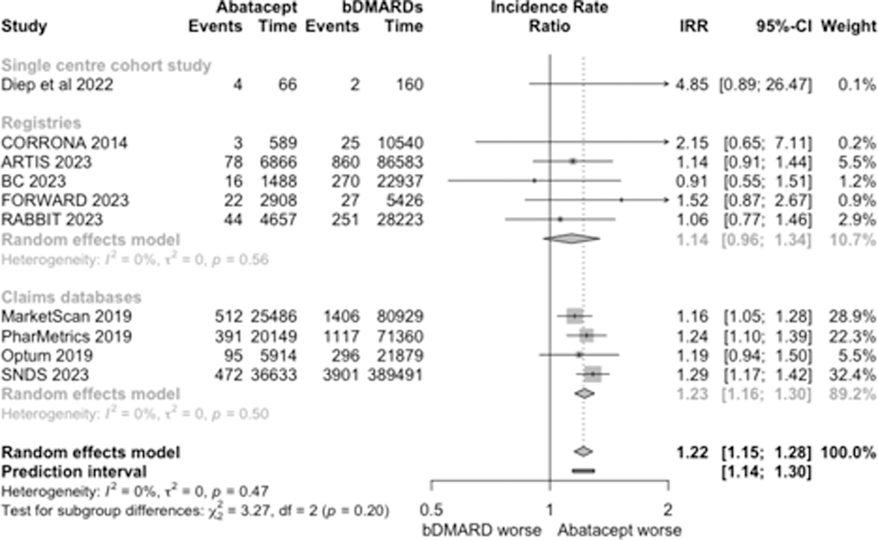
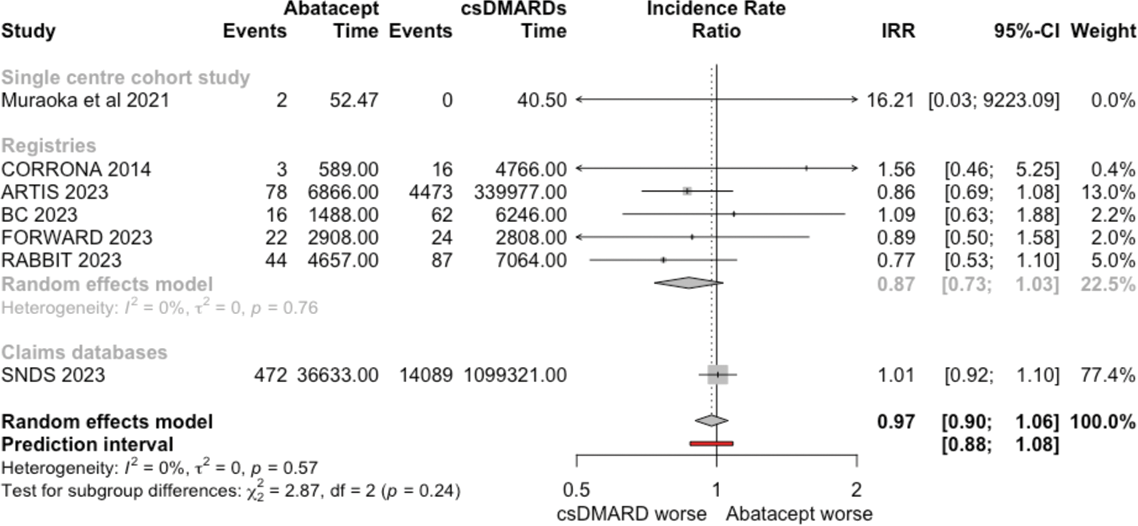
Results: In 14 eligible RCTs and 9 LTE studies, there were 88 malignancies excluding NMSC in 9,958 person-years exposure to abatacept, and 14 malignancies in 1,262 person-years exposure to placebo. The overall malignancy incidence rate with abatacept exposure 8.84 vs. 11.1 with placebo exposure. In observational cohort data (Registries n=5, Claims databases n = 4, Single Centre Cohorts n=1), there were 1,637 malignancies in 104,756 person-years exposure to abatacept (overall malignancy incidence rate 15.6), 8,155 malignancies in 717,528 person-years exposure to other bDMARDs (overall malignancy incidence rate 11.4), and 18,751 malignancies in 1,460,223 person-years exposure to csDMARDs (overall malignancy incidence rate 12.8). In pairwise meta-analysis, there was no significant difference in the risk of malignancy excluding NMSC between abatacept and placebo from combined RCT and LTE data (pooled IRR 0.64; 95% CI 0.35 to 1.18) (Figure 1). In observational cohort data, there was a significantly increased risk of malignancy with abatacept compared with other bDMARDs (pooled IRR 1.21; 95% CI 1.15-1.28) (Figure 2), but no significant difference in malignancy rates between abatacept and csDMARDs (pooled IRR 0.95; 95% CI 0.90 to 1.01) (Figure 2).
Conclusion: There was no significant difference between abatacept and placebo in RCT and LTE data. However, a significantly increased risk of malignancy was observed when compared with other bDMARDs, but not with csDMARDs, in observational cohort data.
Observational data are limited by channelling bias. However, their strength lies in a more generalisable sampling frame and longer per patient duration of follow-up, which is particularly relevant for adverse events with a long latency. Our findings strongly support further pharmacovigilance work to evaluate whether a malignancy risk truly exists with abatacept.
REFERENCES: [1] Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved Survival with Ipilimumab in Patients with Metastatic Melanoma. New England Journal of Medicine. 2010 Aug 19;363(8):711–23.
[2] Simon TA, Dong L, Suissa S, Michaud K, Pedro S, Hochberg M, et al. Abatacept and non-melanoma skin cancer in patients with rheumatoid arthritis: a comprehensive evaluation of randomised controlled trials and observational studies. Ann Rheum Dis. 2023 Nov 6;ard-2023-224356.
Acknowledgements: NIL.
Disclosure of Interests: Benjamin Zuckerman: None declared, Mark Gibson: None declared, Ritika Roy: None declared, Mark Hughes: None declared, Daksh Mehta: None declared, Maryam A. Adas: None declared, Kenrick Ng: None declared, Sam Norton: None declared, Mark Russell: None declared, Andrew Cope Consulting fees from BMS, AbbVie and GSK/Galvini, Grant funding from BMS, James Galloway JG has acted in an advisory role to many pharmaceutical companies (listed below), including to provide specific advice on malignancy risk with JAK inhibition for the purpose of regulatory review. He received no funding for this systematic review and meta-analysis, and there was no industry involvement or oversight for any stage of this project. JG has received honoraria from AbbVie, Biovitrum, BMS, Celgene, Chugai, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfizer, Roche, Sanofi, Sobi and UCB.