

Background: In the follow-up of rheumatoid arthritis (RA) patients, a group of patients who could not reach the treatment target were defined as “difficult to treat” (D2T) by EULAR and in addition to refractory patients in whom inflammatory activity cannot be controlled, cases that are difficult to treat due to psychological and socioeconomic factors are also included in the definition of D2T [1,2]. In addition to RA, it has become important to identify effective factors in D2T cases among other diseases.
Objectives: This study aimed to investigate the reasons for treatment non-response and drug switching in RA, ankylosing spondylitis (AS) and psoriatic arthritis (PSA) patients who have used at least two bDMARD/tsDMARD treatments.
Methods: 110 RA, 70 AS and 34 PSA patients (214 patients in total) who were followed up in the rheumatology outpatient clinic between 2015 and 2023, and had a history of at least 2 bdMARD/tsDMARD use were included in the study. 110 RA patients had 254 drug changes [mean: 3.13 drugs, (2-9)], 70 AS patients had 193 drug changes [mean: 3.6 drugs, (2-9)], and 34 PSA patients had 80 drug changes [mean: 3.21 drugs, (2-7)] were examined retrospectively.
Results: In D2T RA patients, the rate of patients with four or more drug changes was 30.9%, 41% in AS, and 38.3% in PSA. The rate of psychosomatic complaints during medication change is 39.1% in RA, 42.3% in AS and 32.4% in PSA. Surgical treatment disruptions/treatment unresponsiveness were 11.8% in RA, 9.9% in AS and 5.9% in PSA. Drug change/discontinuation due to cancer or cancer risk was 6.4% in RA, 2.8% in AS and 5.9% in PSA. Drug change due to serious infection was 9.1% in RA and 1.4% in AS. Treatment change/disruption due to pregnancy was found to be 7.4% in RA, 6.2% in AS, and 8% in PSA. An increase in disease activity due to lack of follow-up was observed at a rate of 23.6% in RA, 15.5% in AS and 11.8% in PSA. The frequency of refractory patients with regular follow-up and high disease activity despite proper use of the necessary treatment was found to be 15.5% in RA, 16.9% in AS, and 20.6% in PSA. In 12.7% of RA patients, 23.9% of AS patients and 17.6% of PSA patients; upon the patient’s request, treatment switched back to the previously used medication. When the reasons for drug change in RA patients were examined, 35.4% primary non-response, 28.3% secondary non-response, 7.5% allergy/side effects, 5.1% difficulty in administration, 0.8% patient request, 8.7% lack of follow-up, 7.1% serious infections and 81.1% disease activity were found. Reasons for medication changes in AS patients included; 31.1% primary non-response, 37.3% secondary non-response, 6.7% side effects/allergy, 6.2% difficulty in application, 2.6% patient request, 6.2% lack of follow-up, 5.2% serious infection, 78.2% disease activity. In PSA patients; 56% primary non-response, 27.5% secondary non-response, 3.8% side effects/allergy, 2.5% difficulty in application, 1.2% patient request, 3.8% lack of follow-up, 1.2% serious infection. 91.2% disease activity and 33.8% psychosomatic findings were found as reasons for drug change. Data obtained from RA, AS and PSA patients are presented in Table 1.
Conclusion: In addition to uncontrolled inflammation in D2T patients, non-inflammatory causes (psychosomatic findings, pregnancy, surgery and lack of follow-up, etc.) also play an important role. Follow-up of D2T patients should also include elements such as patient education, support in special situations, treatment of psychosomatic complaints, and prioritizing “sustainability” in treatment selection.
REFERENCES: [1] Nagy G, Roodenrijs NMT, Welsing PM, et al. EULAR definition of difficult-to-treat rheumatoid arthritis. Annals of the Rheumatic Diseases. 2021 Jan;80(1):31-35. DOI: 10.1136/annrheumdis-2020-217344. PMID: 33004335; PMCID: PMC7788062.
[2] Nagy G, Roodenrijs NMT, Welsing PMJ, et al. EULAR points to consider for the management of difficult-to-treat rheumatoid arthritis. Ann Rheum Dis . 2022;81(1):20-33. doi:10.1136/annrheumdis-2021-220973.
Table 1. Comparative presentation of reasons for medication change in RA, AS and PSA patients.
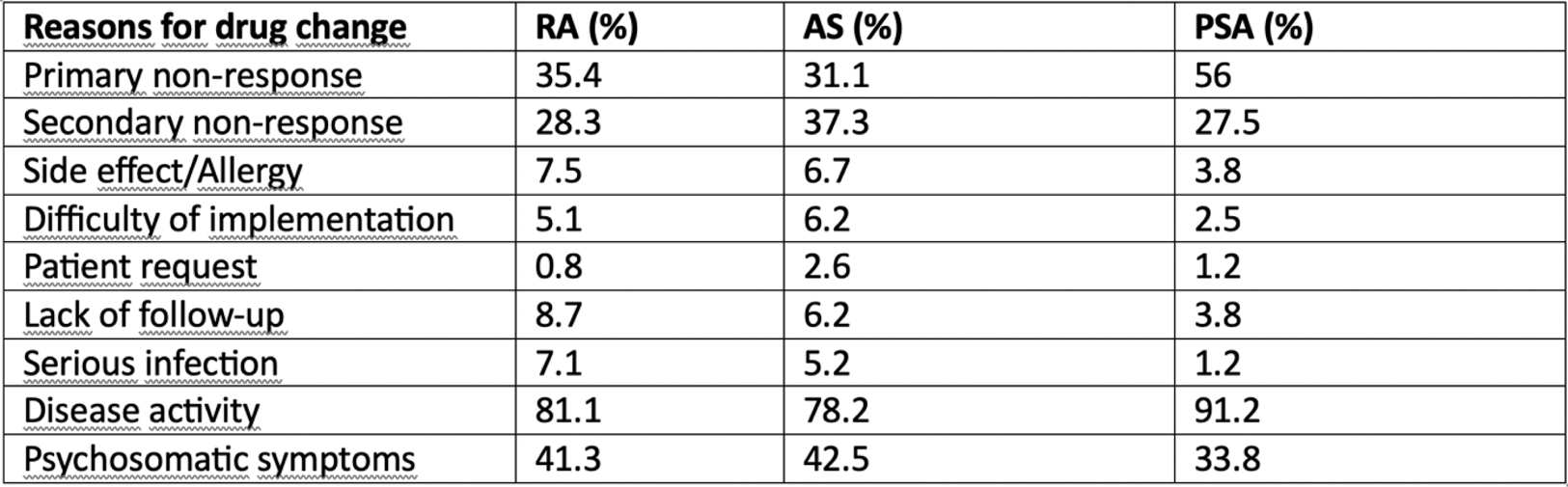
(RA: Rheumatoid Arthritis, AS: Ankylosing Spondylitis, PSA: Psoriatic Arthritis)
Acknowledgements: NIL.
Disclosure of Interests: None declared.