

Background: Glucocorticoids (GCs) are essential immunosuppressive agents used to treat various autoimmune rheumatic diseases (AIRDs), yet are associated with increased risk of infections in a dose-dependent manner.
Objectives: We aimed to develop a model and scoring system to predict serious infections among AIRD patients treated with prolonged, high-dose GCs.
Methods: Data for model development were obtained from a registry of AIRD patients who received high-dose GCs (≥ 30 mg/day with prednisolone equivalent dose) for at least 4 consecutive weeks in Seoul National University Hospital (i.e. derivation cohort). A total of 1635 patients in the derivation cohort were analysed in this study. The primary outcome was occurrence of serious infections requiring intravenous antimicrobials or hospitalization for treatment. The incidence of serious infections over one year after the prolonged, high-dose GC therapy was evaluated. Cox proportional hazards models were used to identify predictors of the primary outcome in the derivation cohort. Next, a scoring system was developed based on beta coefficients of each covariate included in the final model. This scoring system was validated using an independent cohort in Seoul National University Bundang Hospital (i.e. validation cohort, n = 672).
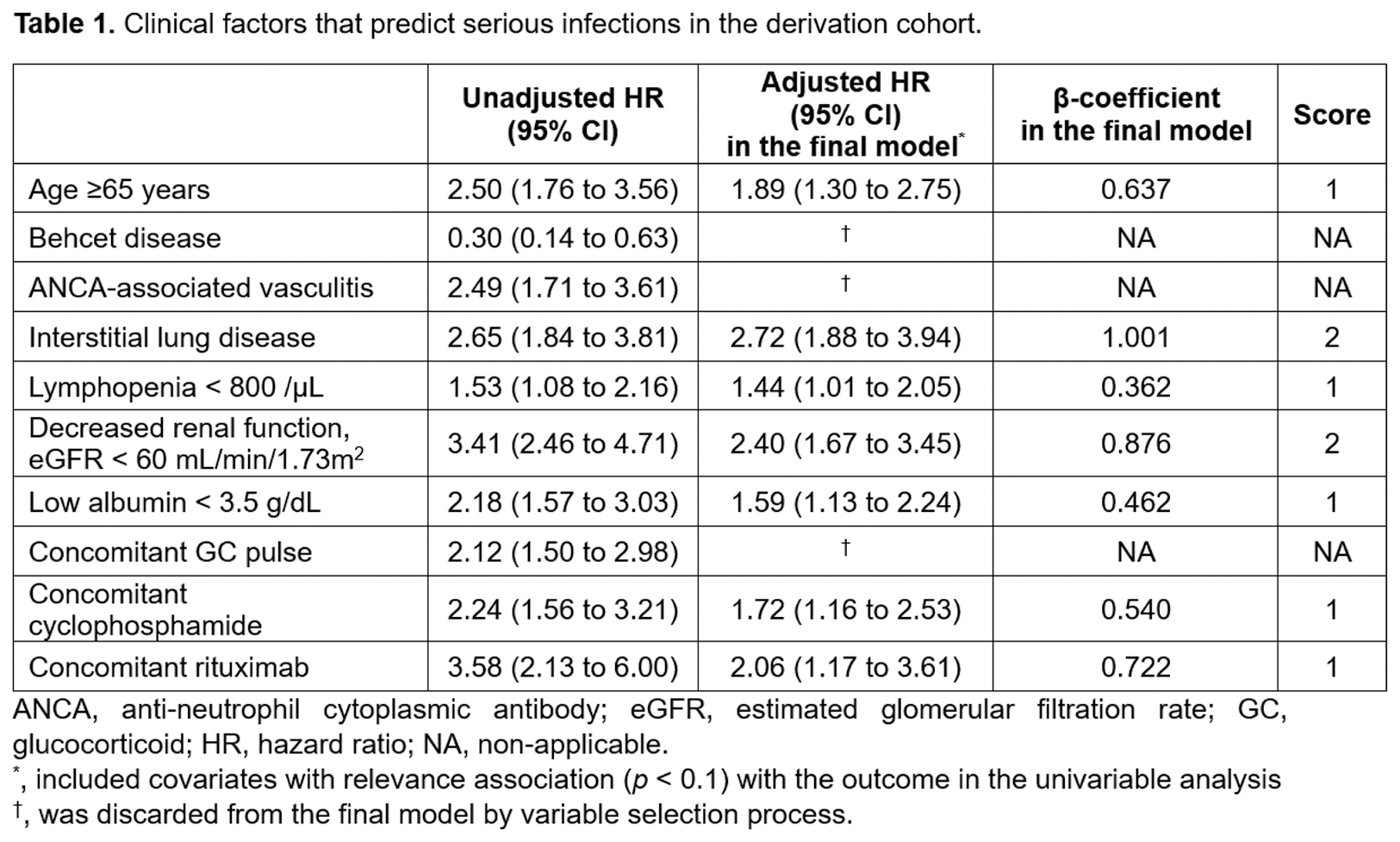
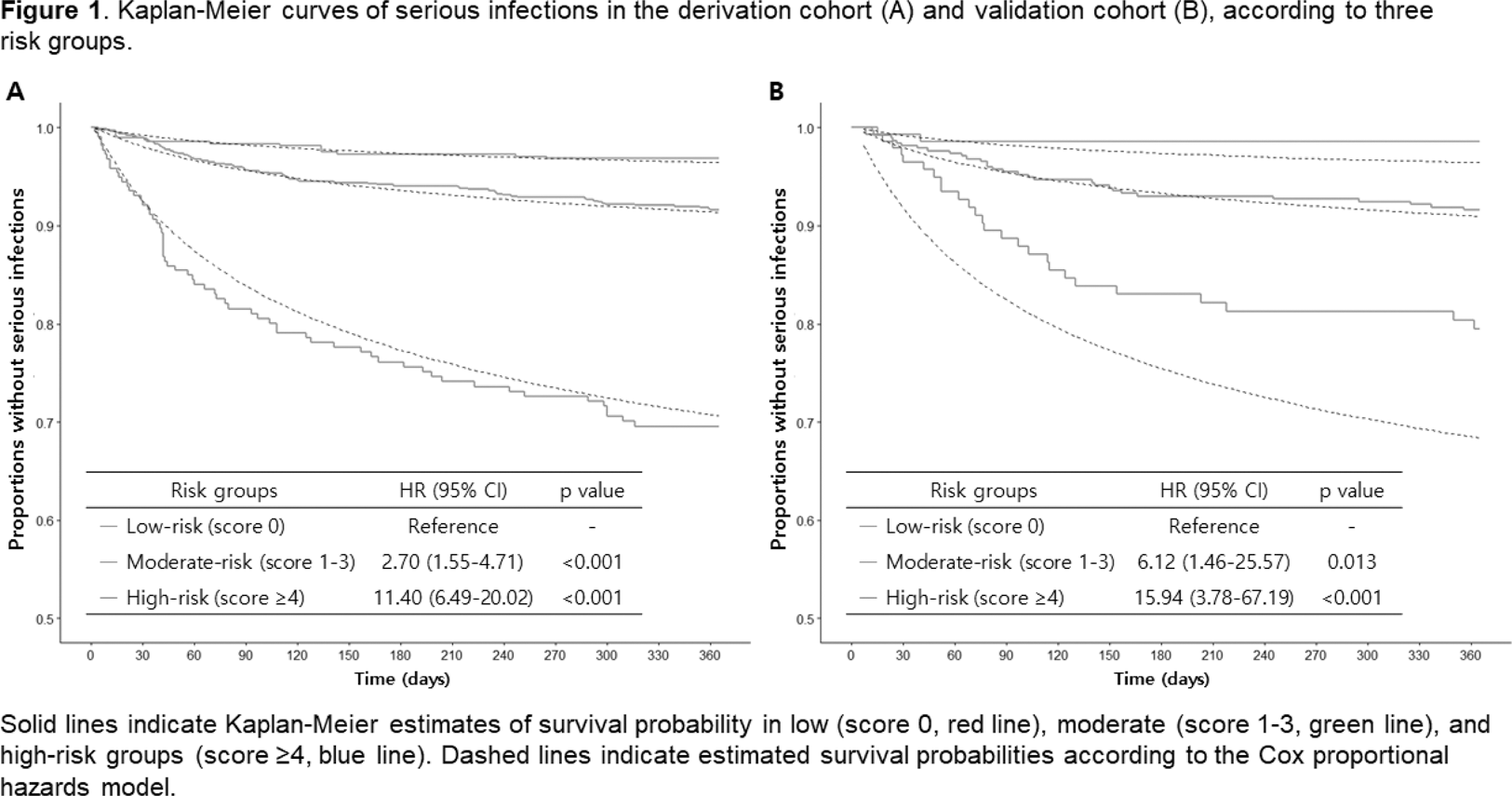
Results: In the derivation cohort, a total of 153 patients experienced serious infections, with an incidence rate (IR) of 10.5 [95% confidence interval (CI) 8.9-12.3] per 100 person-years. The final prediction model included old age ≥65 (adjusted hazard ratio (aHR) 1.89 [95% CI 1.30-2.75], point 1), interstitial lung disease (aHR 2.72 [1.88-3.94], point 2), lymphopenia (aHR 1.44 [1.01-2.05], point 1), decreased renal function (defined as estimated glomerular filtration rate < 60mL/min/1.73m 2 ) (aHR 2.40 [1.67-3.45], point 2), low serum albumin level (aHR 1.59 [1.13-2.24], point 1), concomitant cyclophosphamide use (aHR 1.72 [1.16-2.53], point 1), and rituximab use (aHR 2.06 [1.17-3.61], point 1) (Table 1). According to the predictive risk, patients were classified into three groups; low (score 0), moderate (score 1-3), and high-risk group (score ≥4). IRs [95% CIs] of serious infections in these risk groups were 3.3 [1.9-5.4], 9.0 [7.1-11.3], and 40.1 [30.8-51.3] per 100 person-years, respectively (Figure 1A). The performance of the scoring system was also comparable in the validation cohort (Figure 1B). Harrell’s C-index of the final multivariable model was 0.720 in the derivation cohort and 0.719 in the validation cohort, indicating excellent discrimination performance.
Conclusion: The established novel scoring system accurately predicted the risk of serious infection in patients with AIRDs receiving prolonged, high-dose GCs.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.