

Background: The transfer of anti-Ro antibodies through the blood-placental barrier during pregnancy and its relation to development of congenital heart block and neonatal lupus erythematosus is widely described. Nevertheless, there are fewer data about the features of patients with anti-Ro antibodies and its impact on the outcome of pregnancy.
Objectives: The aim of the study was to describe the characteristics of the patients and the outcome of pregnancy assessed in a specific pregnancy multidisciplinary team.
Methods: Retrospective study of patients with anti-Ro antibody-positivity with follow-up in a multidisciplinary rheumatology-obstetrics and gynecology consultation in Madrid (Spain) from December 2012 to January 2023. Patients that were included may have an associated disease. Each episode of preconceptional counseling was established as a case. Categorical variables were described as proportions and/or percentages, while continuous variables were shown as mean and standard deviation (SD). The Student t test and χ2 test were used to compare data (anti-Ro-60, anti-Ro52, anti-Ro-60/52 groups) when appropriate.
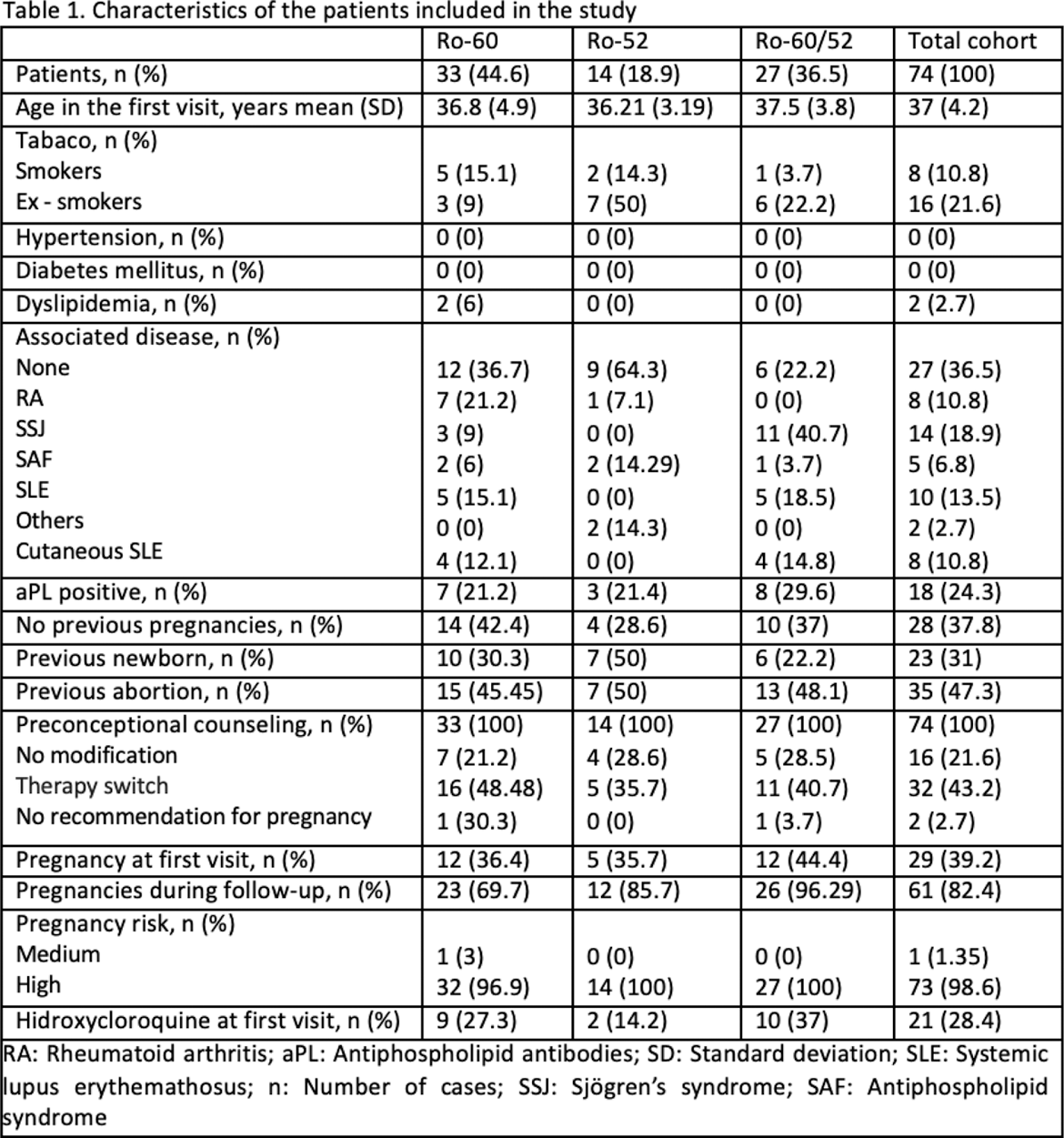
Results: 74 cases were included, 33 of which (44.6%) were positive for anti-Ro60 antibodies, 14 for (18.9%) anti-Ro52 and 27 (36.5%) were positive for both. For each case, we took the principal characteristics, presented in Table 1.
The average age on the first visit was 37 years old. The most prevalent disease described was Sjögren syndrome (18.9%), followed up by Systemic Lupus Erythematosus (13.5%). 36.5% of the patients did not present any associated disease. 98.6% of pregnant women were considered at “high risk”.
Preconceptional counseling consisted of a therapy switch in 43.2% of the cases, remaining the same in 21.6% of the cases. In 2.7% of women pregnancy was discouraged. 28.4% of the patients were already treated with hydroxycloroquine and its introduction was recommended in 63.5%.
The pregnancy rate was 82.4% (61/74). 9 out of 61 (14.7%) pregnant women had an abortion. In our cohort, the proportion of life birth rate was 82% (50/61). 82% (50/61) of pregnant women had full-term births of which 50% (25/50) were eutocic deliveries and 26% (13/50) caesarean sections carried out at 39.2 weeks of gestation on average.
From 50 full-term births, 88% (44/50) were on treatment with hidroxycloroquine and there were 5 (10%) outbreaks of the mother’s rheumatic or autoimmune underlying disease, one in the first trimester, two in the second one and other two in the third one. A fetal ultrasound monitoring each two weeks was made between 16 and 26 weeks of pregnancy in every patient, without noticing any case of congenital heart block.
Adverse obstetrical and neonatal outcomes were observed. The most frequently recorded outcome was gestational diabetes (50%) followed up by prelabour rupture of the membranes (25%) and one case (8.3%) of pre-eclampsia. 25% of newborns presented low birth weight. In our cohort, none of the newborns developed neonatal lupus erythematosus. None of the anti-Ro antibody positive patients developed a connective tissue disease after pregnancy.
Conclusion: Our study shows that 36.5% of patients with anti-Ro antibodies did not present an underlying associated disease. Furthermore, treatment with hydroxychloroquine was widely used during pregnancy. In our cohort, no cases of congenital heart block and neonatal lupus erythematosus were observed.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.