

Background: Psoriatic arthritis is a chronic inflammatory disease. These patients have increased risk of developing cardiovascular (CV) events due to disease characteristics. While reducing low-density lipoprotein cholesterol (LDL-C) remains a primary focus in CV disease prevention, it’s important to consider LDL-C subfractions, such as small dense LDL (sdLDL). Even when overall LDL-C levels are within the normal range, sdLDL has been reported to be elevated in chronic inflammatory conditions. The association of CV disease with sdLDL is noteworthy, as these particles possess the capacity to penetrate the arterial wall, increasing susceptibility to oxidation (1). There is a lack of information regarding the association of sdLDL and atherosclerotic disease in PsA patients.
Objectives: We aimed to evaluate the association between sdLDL and subclinical atherosclerosis in PsA patients.
Methods: We recruited a total of 109 consecutive patients with PsA diagnosis according to 2006 CASPAR classification criteria, aged ≥18 years. Patients with a previous CV event, another connective tissue disease or pregnancy were excluded. A carotid ultrasound was performed to all patients, and the presence of carotid plaque (CP) was considered as a carotid intima media thickness (cIMT) ≥ 1.2 mm or a focal narrowing ≥ 0.5 mm. A blood sample was drawn to measure a lipid profile. We calculated sdLDL with the following formula: 0.580 [non–high density lipoprotein (HDL-C)] + 0.407 (direct LDL-C) – 0.719 (calculated LDL-C) – 12.05, where calculated LDL-C = Total cholesterol (TC) – HDL-C – (Triglycerides/5) (2). Patients were divided in two groups, with and without CP. Comparisons were done with Chi-square test, Student’s T test and Mann-Whitney’s U test. Correlations between cIMT and lipid profile were performed with Spearman’s correlation coefficient (rs). A p -value < 0.05 was considered statistically significant.
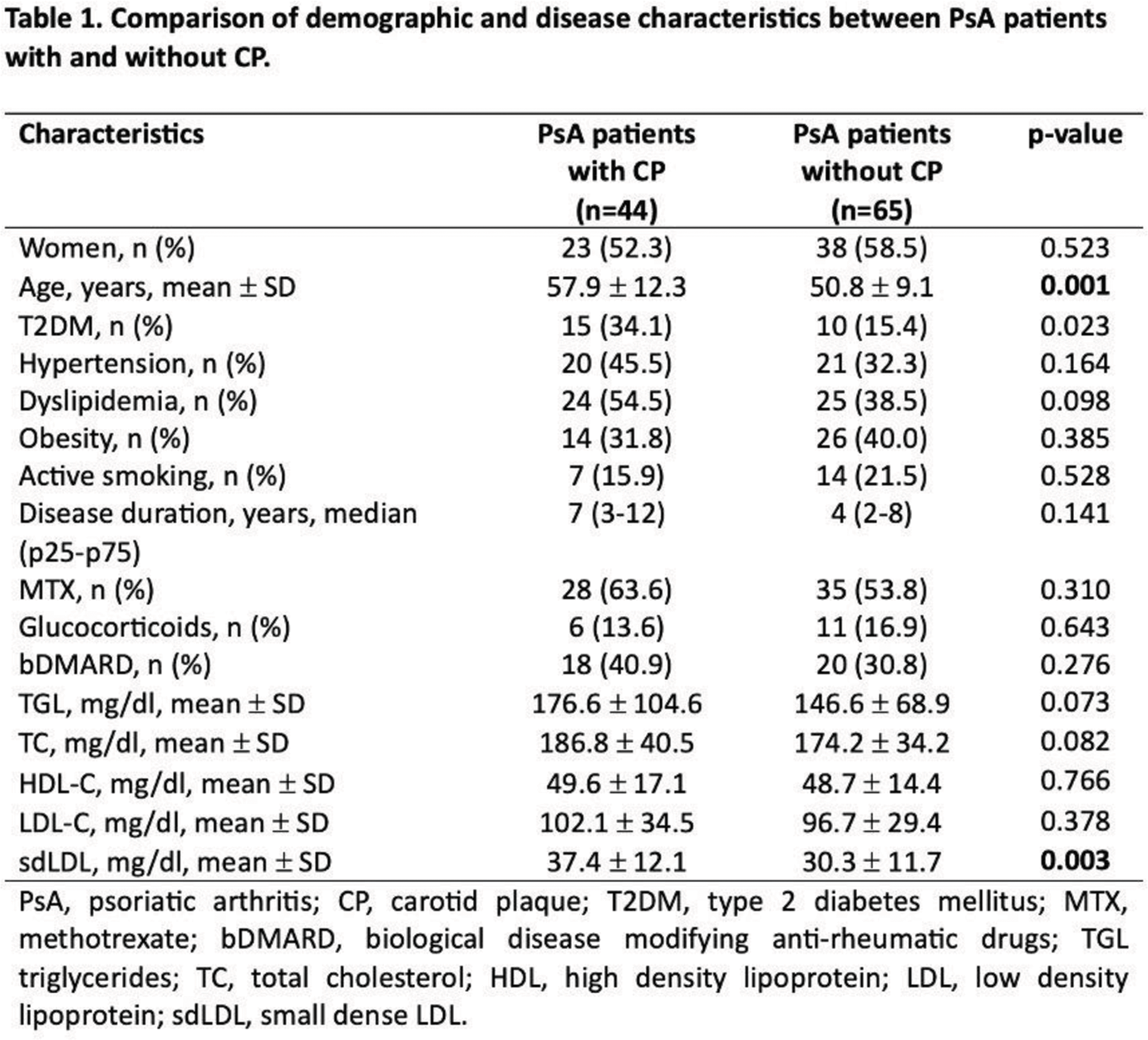
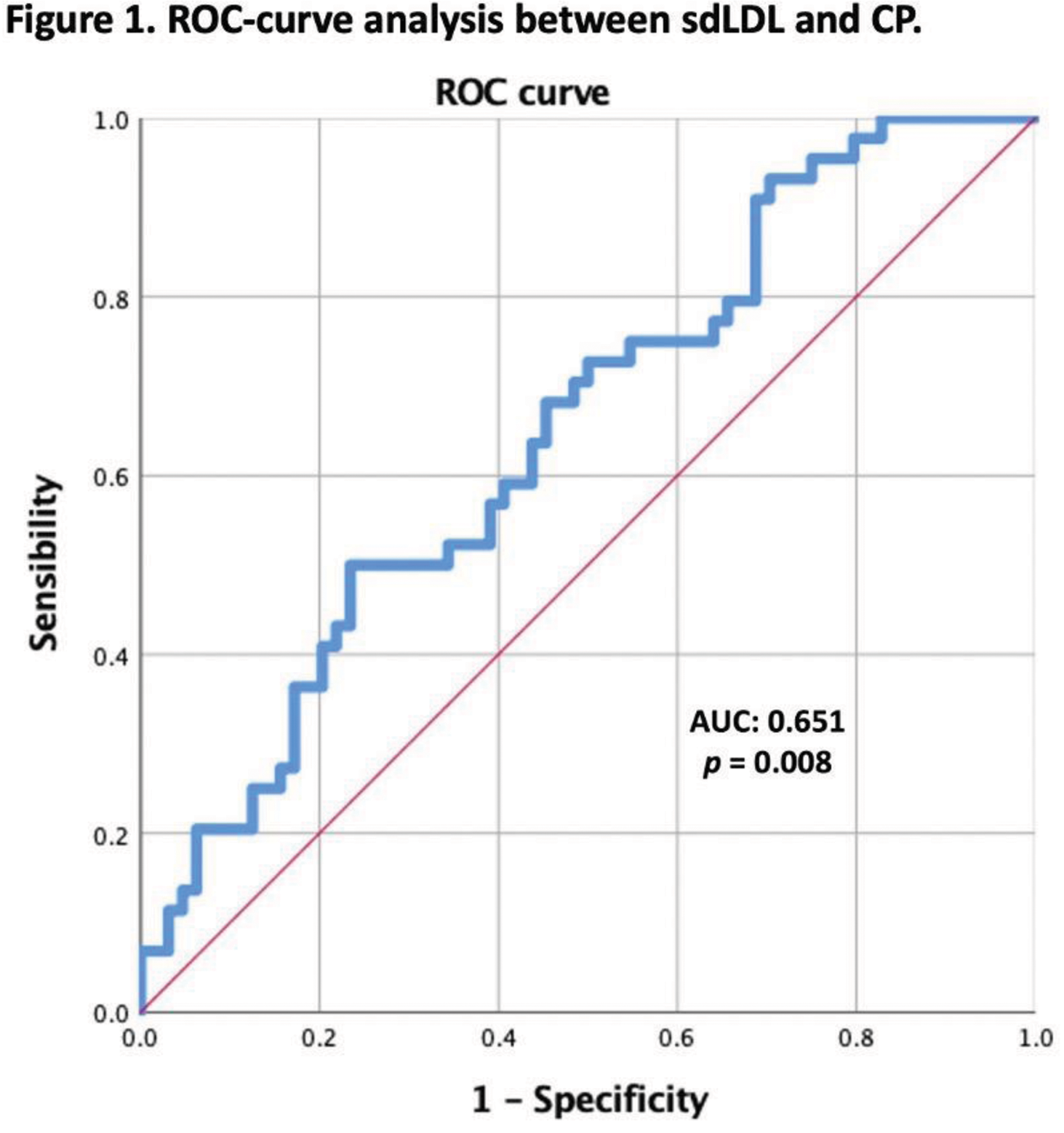
Results: Comparisons between both groups showed that PsA patients with CP were older (57.9 years vs 50.8 years, p = 0.001), had higher prevalence of type 2 diabetes mellitus (34.1% vs 15.4%, p = 0.023), and had increased sdLDL (102.1 mg/dl vs 96.7 mg/dl, p = 0.003). When comparing the rest of the lipid profile no significant differences were found (Table 1). In the univariate analysis we identified a moderately positive correlation between sdLDL and cIMT (rs = 0.305, p = 0.001), and a low positive correlation between TC and cIMT (rs = 0.199, p = 0.038). Correlations with the rest of the lipid profile were not significant. Subsequently, a multivariate analysis, adjusted for age and TC, revealed that elevated sdLDL is independently associated with increased cIMT, with a β = 0.007 (95% CI 0.002-0.012, p = 0.012). Finally, a ROC-curve analysis of sdLDL and CP showed an AUC 0.651 (95% CI 0.547-0.754, p = 0.008), with a cutoff point of 32.3, a sensibility of 63.6% and a specificity of 56.2% (Figure 1).
Conclusion: This study revealed a significant association between sdLDL and subclinical atherosclerosis in patients with PsA. Elevated sdLDL levels were observed in patients with CP, and these increased levels were independently linked to higher cIMT. Interestingly, the conventional lipid profile did not demonstrate a comparable association with atherosclerosis. Furthermore, sdLDL demonstrated a specific capability to identify PsA patients with CP. Given these findings, the measurement or calculation of sdLDL should be incorporated into the routine CV risk assessment for PsA patients.
REFERENCES: [1] Sorokin AV, Patel N, Li H, Hong CG, Sampson M, O’Hagan R, et al. Estimated sdLDL-C for predicting high-risk coronary plaque features in psoriasis: a prospective observational study. Lipids Health Dis. 2023 Apr 27; 22(1):55.
[2] Palazhy S, Kamath P. Estimation of Small, Dense LDL Particles Using Equations Derived From Routine Lipid Parameters as Surrogate Markers. Biochemistry & Analytical Biochemistry. 2014; 3(1).
Acknowledgements: NIL.
Disclosure of Interests: None declared.