

Background: Glucocorticoids (GC) are central to the treatment of rheumatic diseases such as systemic lupus erythematosus and vasculitis syndromes, and are also used in the treatment of diseases in other areas. However, their systemic effects, especially glucocorticoid-induced osteoporosis (GIOP), represent a significant but preventable side effect.
Objectives: Our tertiary care institution embarked on a quality improvement initiative aimed at improving the prevention and treatment of GIOP and addressing its under-recognition and suboptimal management.
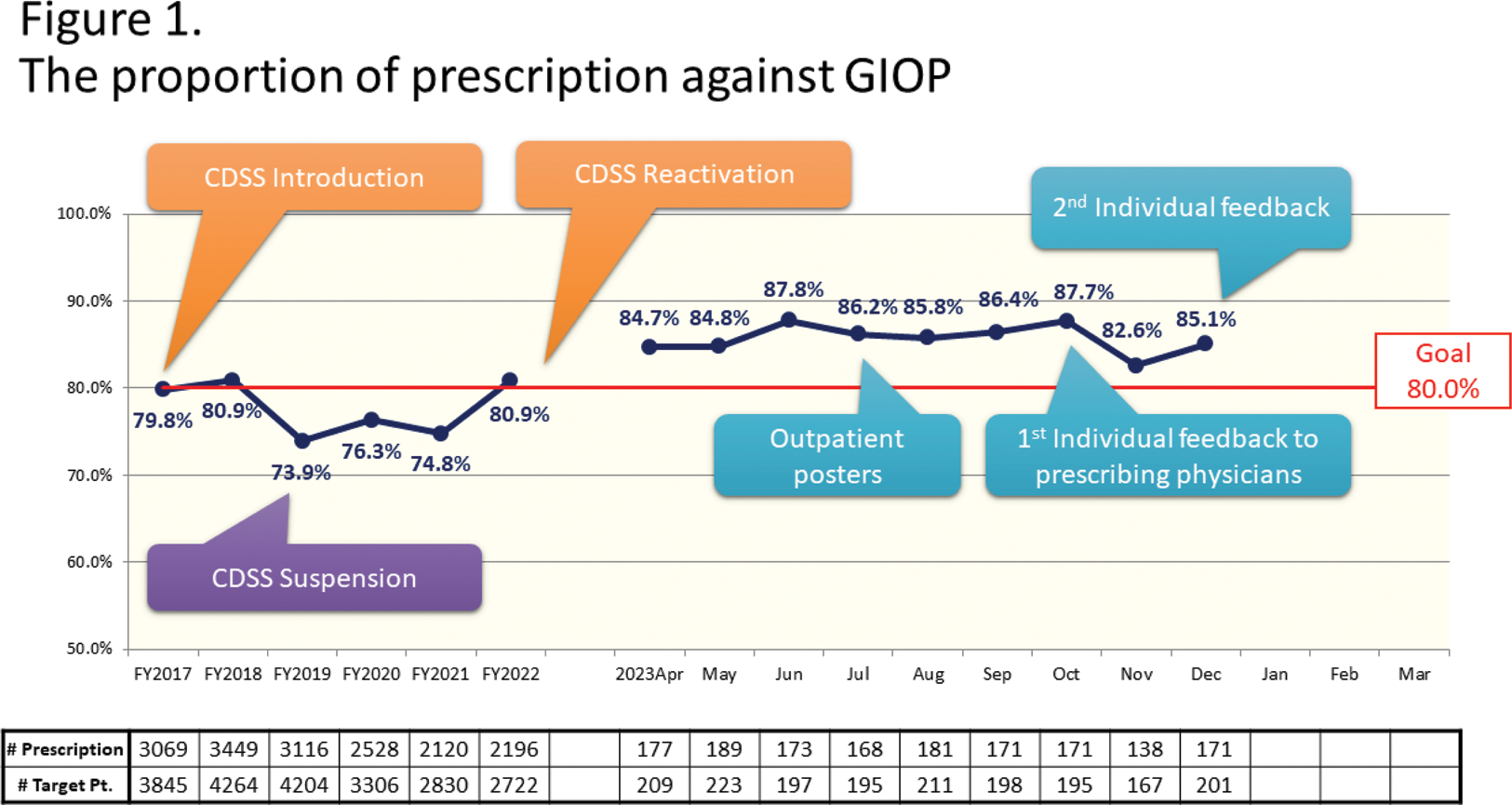
Methods: Since 2011, we have been using the prescription proportion of osteoporosis medication for GIOP as a quality indicator.[1] Currently, patients taking GC equivalent to prednisolone 2.5 mg or more daily for over three months were targeted according to recent ACR guideline [2], aiming for a QI target of 80%. Patients younger than 18 years old, using GC for an intermittent use due to bronchial asthma attacks or other disease flare, recent eGFR less than 60, kidney stone disease, hypercalcemia, pregnancy, lactation, any other contraindications to each osteoporosis medication etc., were excluded. A clinical decision support system (CDSS), introduced in 2017, alerts physicians if their patients are not taking osteoporosis medication and provides a treatment flowchart. The CDSS was temporarily suspended in 2020 for electric health record system updates, but was reactivated in January 2023. In addition, we used educational posters for patients in our outpatient clinic from July 2023 and individualized feedback to physicians to maintain QI in October and December 2023. The proportion of bone density testing (DEXA scan) within one year in the same patient group was also tracked.
Results: From 2017, 2730-4264 patients in total were included annually. Until 2022, the QI fluctuated around 80%, but since the CDSS reactivation in 2023, it has consistently exceeded 80% (Figure 1).
The proportion of bone density testing has generally maintained above 60% in FY2023 (Figure 2).
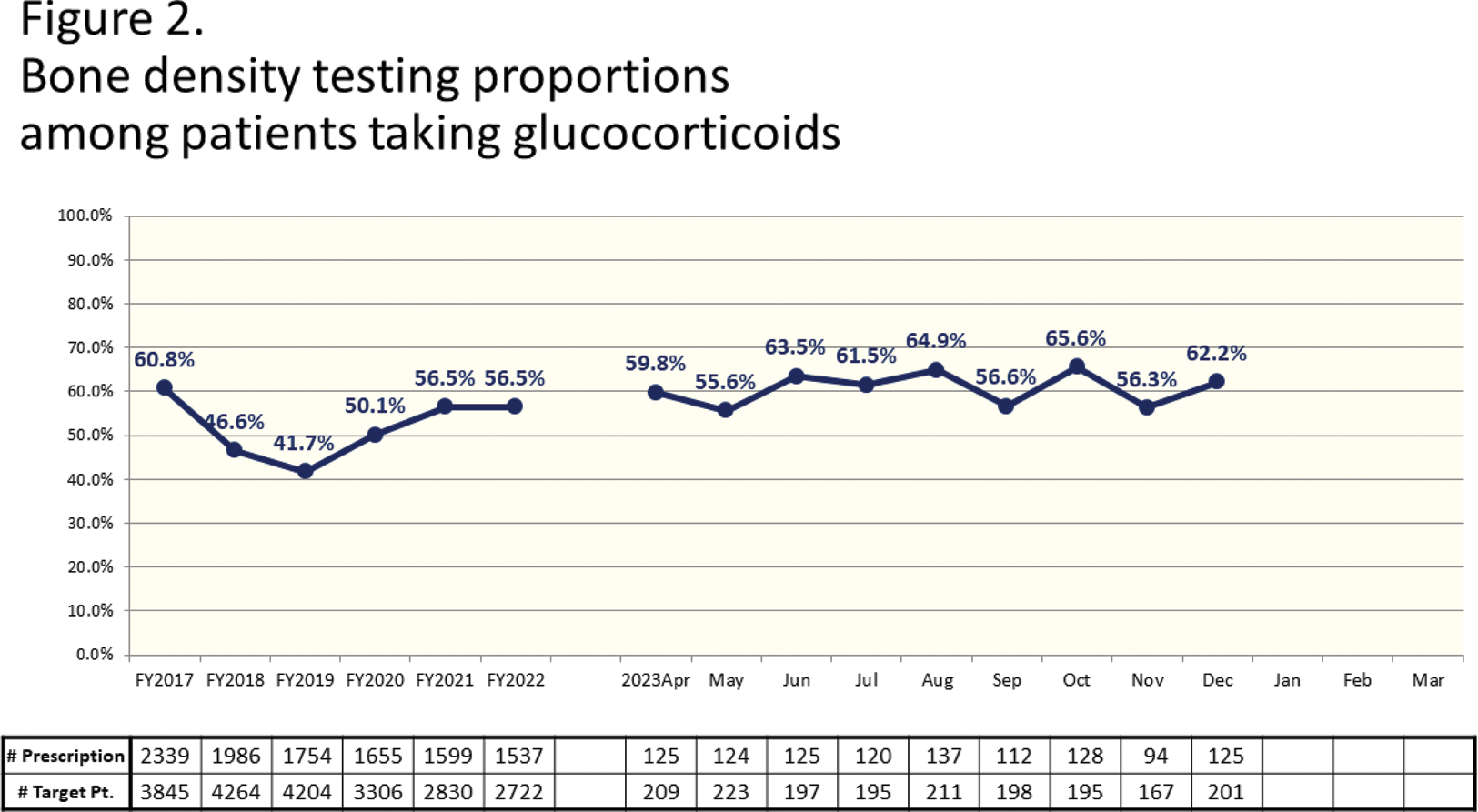
Conclusion: CDSS reactivation has shown a positive correlation with improved QI, indicating its effectiveness in reducing prescription omissions and disseminating treatment strategies. However, the non-response of some physicians to CDSS alerts highlights the need for additional strategies, including patient education and direct physician feedback. Future plans include integrating bone density test reminders into the CDSS to further optimize treatment decisions for GIOP.
REFERENCES: [1] SUDA, Masei, et al. Effects of quality indicator monitoring for glucocorticoid-induced osteoporosis and trends of drug treatment in a Japanese hospital. International Journal of Rheumatic Diseases , 2018, 21.5: 975-981.
[2] HUMPHREY, Mary Beth, et al. 2022 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis. Arthritis & Rheumatology , 2023, 75.12: 2088-2102.
Acknowledgements: NIL.
Disclosure of Interests: None declared.