

Background: Rates of total knee arthroplasty (TKA) in the United States have risen, coupled with increasing demand for TKAs in younger patients. [1] Although rates of postoperative complications in TKA have decreased significantly, [2] they remain a significant concern for patients and clinicians.
Objectives: In light of these changing trends in TKA use and outcomes, we sought to understand how risk for adverse TKA outcomes changes with age using machine learning algorithms.
Methods: We studied patients undergoing TKA from the Pennsylvania Health Care Cost Containment Council (PHC4) Database, 2012-2018. Our primary variable of interest was age as a risk factor for the binary outcomes of 90-day readmission, 90-day mortality, 1-year revision, and the continuous outcome length of stay (LOS). Our model included patient-level demographics and covariates, including sex, race, discharge location, and insurance. We trained explainable boosting machines (EBMs) to predict risk (70% train:30% test) for the aforementioned outcomes. [3] For binary outcomes, we stratified the training data by outcome for balance. EBMs are highly accurate, interpretable models that are flexible in visualizing the dependent variables and handle collinearity well which is important in TKA. We report test AUROCs and R 2 as evaluation metrics for predictive performance of the models, and further include partial dependency plots which explain the relationship of age with these outcomes.
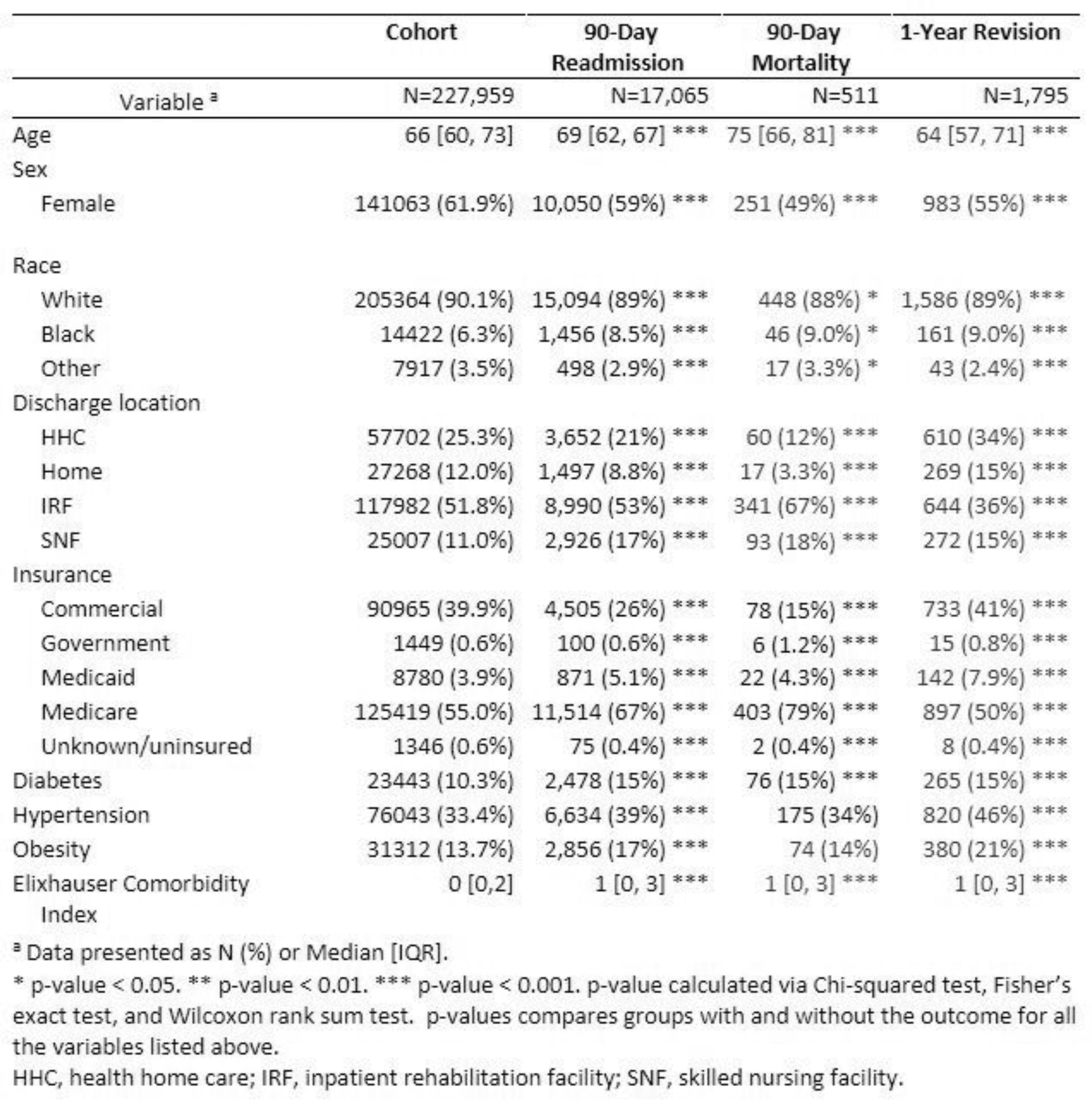
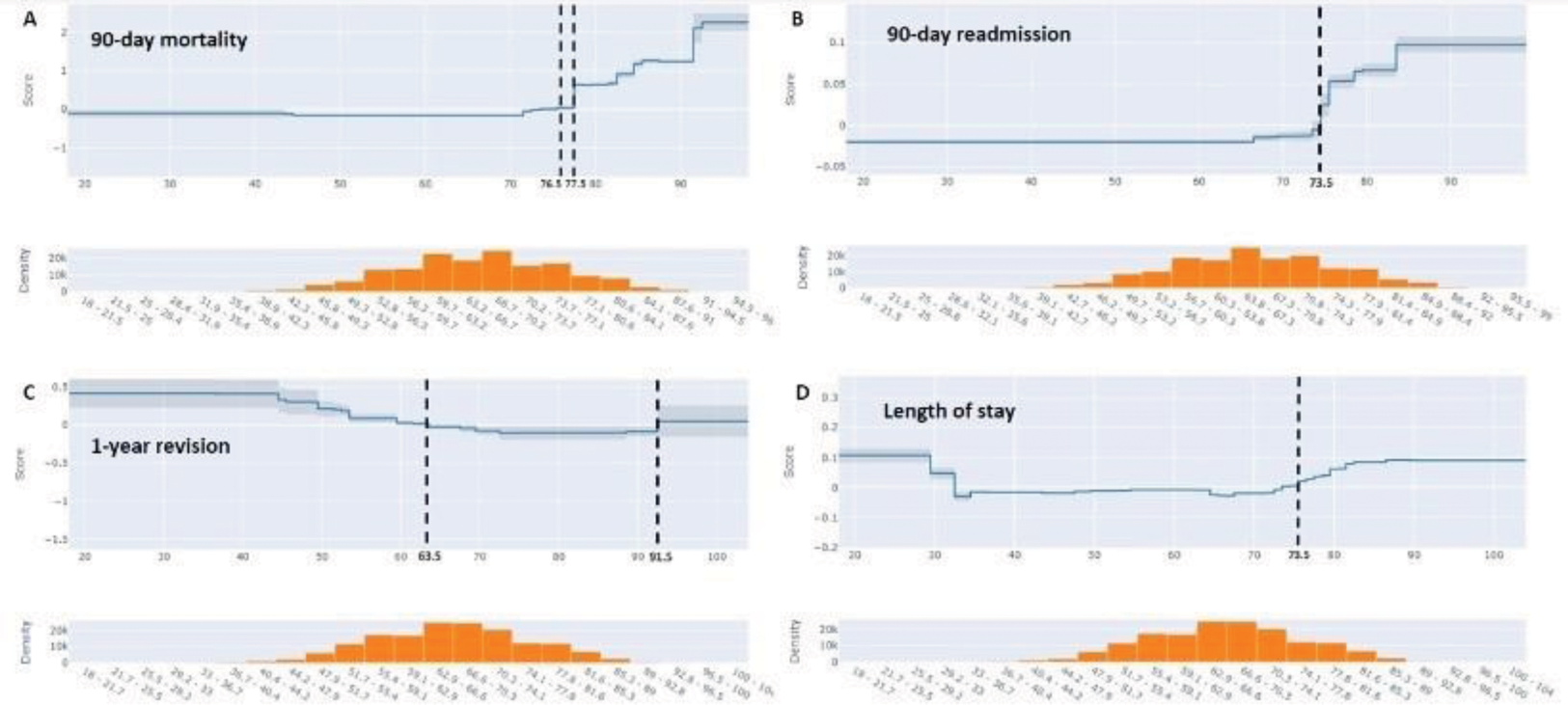
Results: We had a cohort of 227,959 TKA patients, with a median age of 65 years with 90.1% White and 55% Medicare-insured (Table 1). 90-day readmission was observed in 7.49%, 90-day mortality in 0.22%, and 1-year revision in 0.79%. Predictive performance of adverse outcomes was strongest for 90-day mortality (AUROC=0.74), followed by 1-year revision (AUROC=0.64), 90-day readmission (AUROC=0.62), and LOS (RMSE=0.36, R 2 =0.13). Age was among the most important factors for predicting all outcomes and its relationship with the outcomes is detailed in the partial dependency plots in Figure 1. Predicted risk of 90-day mortality increases significantly after the age of 77.5 years, whereas 90-day readmission increases after the age of 73.5 years, and LOS risk increases at 73.5 years. However, with 1-year revision the risk decreases after the age of 63.5 (Figure 1).
Conclusion: We determined that the effect of age as a risk factor for poor TKA outcomes changes dramatically at specific time points, thus demonstrating that there is a nonlinear relationship between age and TKA outcomes. Traditional regression models have always been understood to have a proportionate increase in risk as age increases. However, our study gives nuance to this understanding and can help physicians and patients in decision-making when trying to quantify risks related to aging as they consider TKA as a treatment option.
REFERENCES: [1] Ravi B et al. The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. PMID:23218428
[2] Singh JA et al. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. PMID:30988126
[3] Nori H et al. InterpretML: A Unified Framework for Machine Learning Interpretability. arXiv:1909.09223
Table 1.
Acknowledgements: The authors would like to acknowledge the Anna Marie and Stephen Kellen Foundation for the Kellen Scholar Program.
Disclosure of Interests: Bella Mehta Research support from Novartis, Yi Yuan: None declared, Chloe Heiting: None declared, Kaylee Ho: None declared, Susan Goodman Dr. Goodman reports receiving research and grant support from Novartis and NIH., Peter Sculco Dr. Sculco reports consultancy for DePuy Sythes, EOS Imaging, Intellijoint Surgical, Lima Corporate, and Zimmer Biomet, Fei Wang: None declared, Said Ibrahim: None declared, Peter Cram: None declared, Rich Caruna: None declared