

Background: IL-16 is an immunomodulatory cytokine which has recently been described as a promising urinary biomarker of active proliferative lupus nephritis (LN)[1,2]. Its expression in other types of renal disease remains unexplored, thus it is of interest to further characterize the biomarker potential of IL-16 in other types of autoimmune kidney disease.
Objectives: To investigate IL-16 expression in urine, plasma, and renal tissue in patients with renal IgA vasculitis (IgAV) and thrombotic microangiopathy (TMA) with kidney involvement and compare the findings to population controls.
Methods: 14 patients with IgAV and 26 patients with TMA were included. The histopathological diagnosis was confirmed in all cases by kidney biopsy performed in clinical routine. All TMA patients were diagnosed with a systemic autoimmune disease. Twenty-one patients (81%) had SLE, out of whom 11 (52%) had secondary anti-phospholipid syndrome (APS). Two patients had primary APS, one systemic sclerosis, one polymyositis, and one other systemic inflammatory condition.
Plasma samples were available in all, and urine in 8 IgAV and 4 TMA patients. IL-16 levels in plasma (p-IL-16) and urine (u-IL-16) were measured using ELISA (detection limit 10 pg/mL). Clinical data was collected from medical files. For comparisons, previous data 1 of p- and u-IL-16 from 31 population controls matched for age and sex were included.
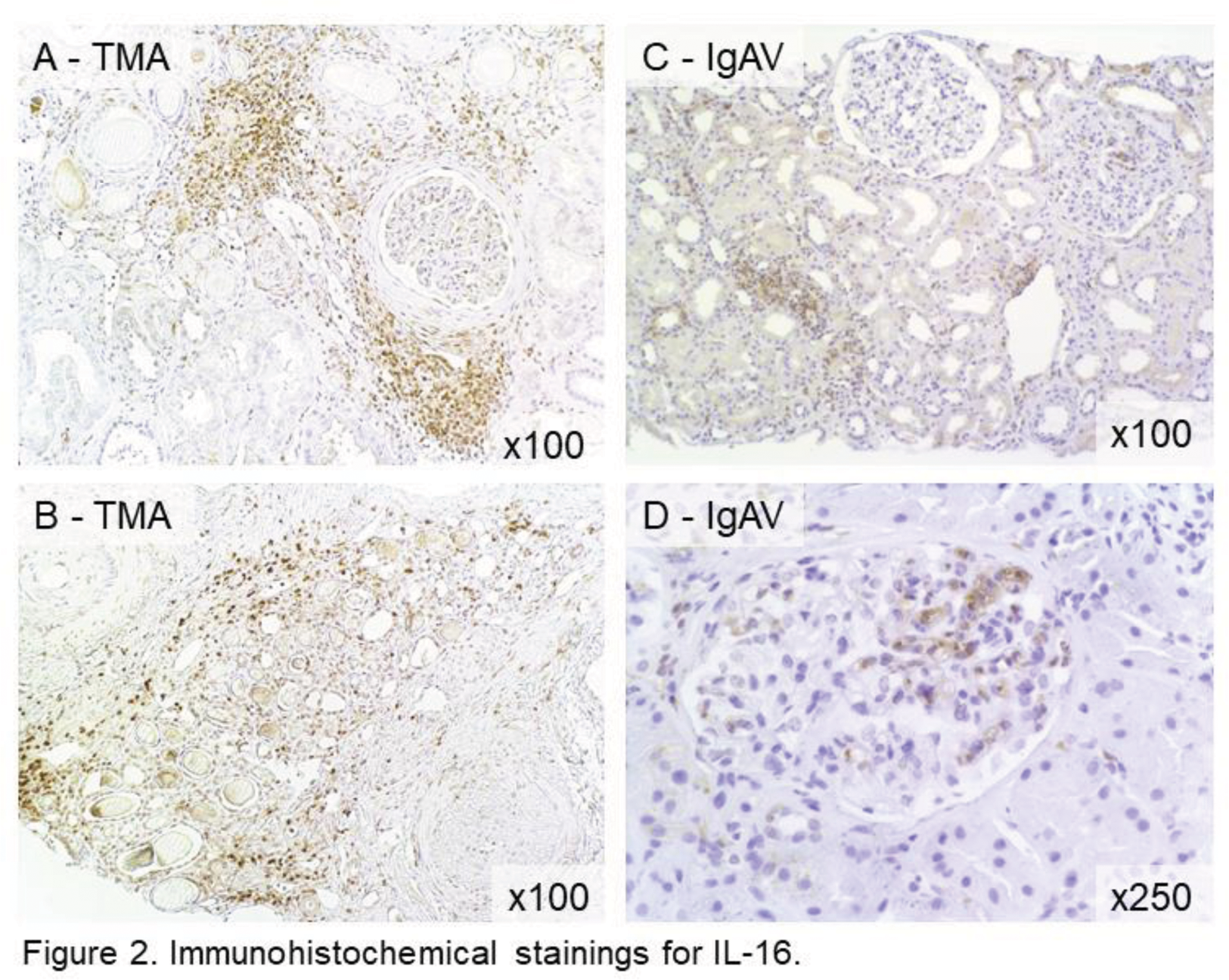
Renal IL-16 expression was studied by immunohistochemistry (IHC) in kidney biopsies of 2 patients with SLE-associated triple-positive APS and TMA but no histopathological signs of LN, and 4 patients with IgAV.
Results: The percentage of females among IgAV patients was 64%, and among TMA patients 85%. The proportions of those with no ongoing immunosuppressive therapy were 64% of IgAV and 24% of TMA patients.
Sixteen of the 21 SLE patients (76%) had a previous or current diagnosis of biopsy-proven lupus nephritis (LN), and 12 (57%) of the 16 LN cases currently co-occurring with TMA (Ten with ISN/RPS class II or V and two with class IV). The remaining four had findings of pure TMA in the current biopsy.
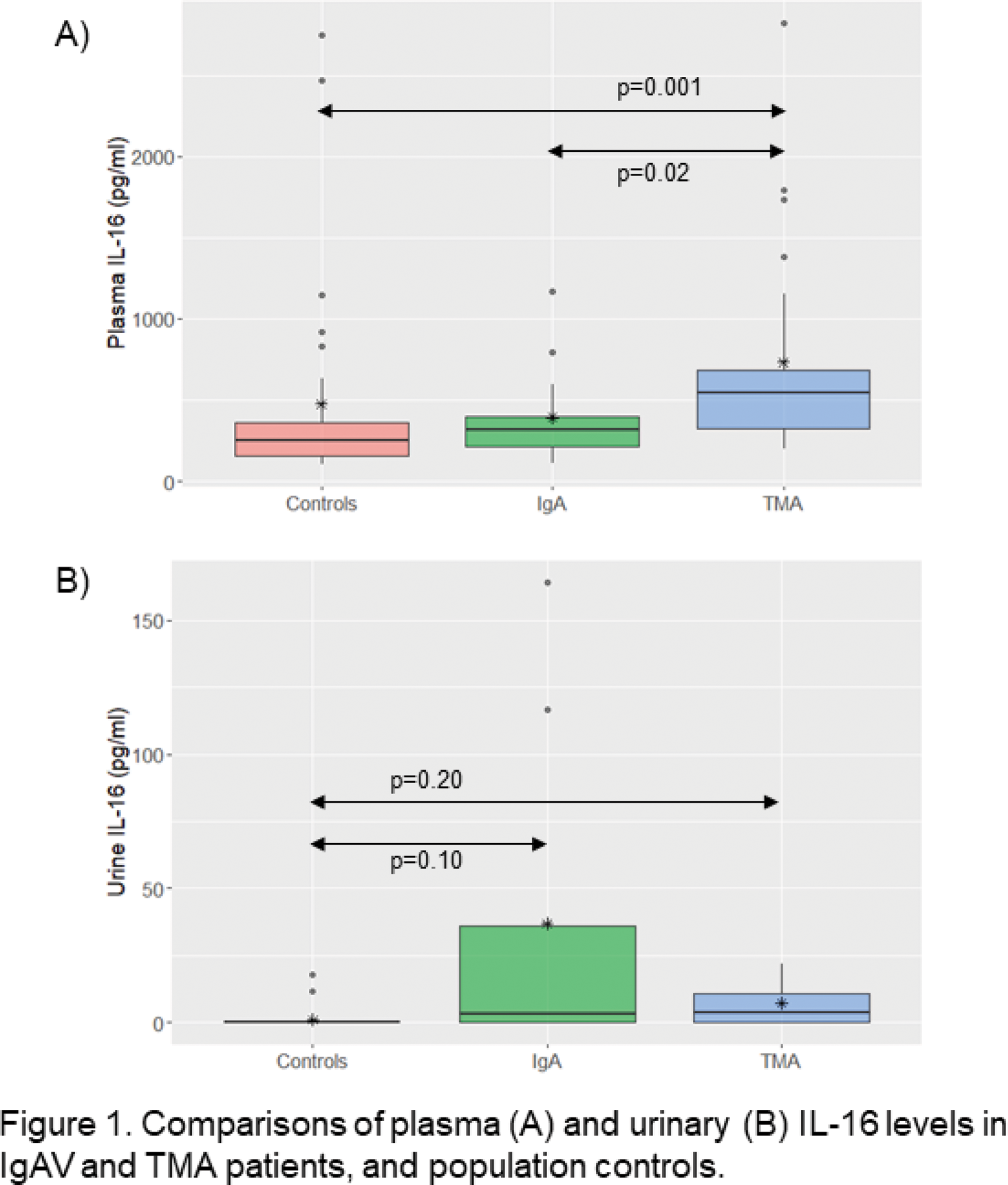
All patients had detectable IL-16 levels in plasma with significantly higher levels in TMA compared to IgAV (median 545 vs 313 pg/mL, p=0.02) and population controls (545 vs 252 pg/mL, p=0.001). No significant difference in plasma levels was observed between IgAV and controls (Figure 1A).
Two out of the eight studied IgAV patients had detectable and high levels of u-IL-16 (116,6 and 164,0 pg/mL respectively). These were the only two patients in the IgAV urine cohort who presented with histopathological findings of cellular glomerular crescents. One TMA patient had detectable u-IL-16 (21,7 pg/mL), however also seen in two of the population controls (11,7 and 17,8 pg/mL). No statistically significant differences were observed in urinary levels between the groups (Figure 1B). No significant correlations between p- and u-IL-16 or u-IL-16 and urine albumin-creatinine ratio were found in IgAV or TMA.
In the immunohistochemical staining, IL-16 was detected in both investigated TMA biopsies, in both cases localized in interstitial inflammatory infiltrates (Figure 2A+B). In the four investigated IgAV biopsies, an interstitial staining was observed (Figure 2C). In two cases of IgAV, a glomerular staining of IL-16 was noted, seen in parallel with necrotic glomerular lesions (Figure 2D). No u-IL-16 levels were available for these patients.
Conclusion: We report increased IL-16 levels in plasma in patients with renal TMA and a trend towards high urinary levels of IL-16 in cases of IgAV, suggesting that IL-16 is involved in the inflammatory process in a wider array of autoimmune kidney diseases. The findings of kidney IL-16 expression, in both conditions, however with different compartments involved, further supports this conclusion. Further studies to confirm the findings are ongoing.
REFERENCES: [1] Häyry, A. et al. Interleukin (IL)-16: a candidate urinary biomarker for proliferative lupus nephritis. Lupus Sci Medicine 2022; 9(1): e000744.
[2] Fava, A. et al. Urine Proteomics and Renal Single Cell Transcriptomics Implicate IL-16 in Lupus Nephritis. Arthritis Rheumatol 2021; 74(5): 829-839.
Acknowledgements: NIL.
Disclosure of Interests: None declared.