

Background: Studies have shown the main cause of atherosclerotic cardiovascular disease (ASCVD) is a combination of low-density lipoprotein cholesterol (LDL-C) and systemic inflammation. Statins have dual action of lipid-lowering and anti-inflammatory, making them an effective treatment for ASCVD. Recommended treatment targets for LDL-C and high-sensitivity C-reactive protein (hs-CRP), as a surrogate for systemic inflammation, are <70mg/dL and <2mg/l, respectively [1,2]. Residual cholesterol risk (RCR) and residual inflammatory risk (RIR) are terms coined by Ridker to describe those who do not achieve these treatment targets despite intensive statin treatment [1,2]. Rheumatologists have a major responsibility to prevent ASCVD, and international guidelines have been published by EULAR/ACR to guide them [3].
Objectives: The objective of this study was to investigate what proportion of patients with rheumatoid arthritis (RA), who were in remission at the last two clinic visits and did not attain achieved the above-stated target levels of LDL-C (<70mg/dl) and hs-CRP (<2 mg/L) and, as a result, remained in the RCR and/or RIR category.
Methods: The study included clinically diagnosed and ACR/EULAR classified patients with RA, who were in complete remission at the last 2 outpatient visits. They had received appropriate DMARD treatment as recommended by international guidelines aiming for ‘remission’ (based upon Simplified Disease Activity Index {SDAI} composite index), along with stringent lipid control using statins, aiming LDL-C level to <70 mg/dL; or total cholesterol/HDL-C ration <3.5. The study excluded patients who had had any form of ASCVD in the past or during the follow-up in this clinic. Multi-morbidities if any were also recorded.
The hospital’s rheumatology department has received approval from the Ethics Committee to conduct clinical data mining for research purposes. The researchers will maintain strict anonymity and have extracted the necessary information into a password-protected Excel sheet.
Results: In this study, 130 patients diagnosed with RA and meeting the aforementioned criteria were included. Table 1 provides demographic information about the study subjects and the duration of their follow-up. Notably, all participants met the ACR/EULAR criteria for remission at the time of their last two follow-up clinic visits. Furthermore, each patient was receiving appropriate treatment with Disease-Modifying Antirheumatic Drugs (DMARDs) as per the ‘treat-to-target’ approach. The results detailing hs-CRP levels and LDL-C are outlined in Table 2. Notably, 91 patients (70%) were categorized as ‘RCR,’ while 81 patients (62%) were classified as ‘RIR.’ Remarkably, these results were observed despite rigorous lipid control measures that included intensive statin therapy, frequently combined with ezetimibe treatment.
Conclusion: This study shows a clear discrepancy between the recommended lower target level of hs-CRP for ASCVD prevention (<2 mg/l) vs. ‘Boolian2 remission in RA’ (≤10 mg/l). Thus, as shown in this study, 60% of RA in Boolean2 remission, were still in ‘RIR’ category for developing ASCVD. Therefore, for stringent ASCVD control in RA, ACR/EULAR may have to re-revise the ‘remission’ criteria down-scaling the upper permissible hs-CRP level of <2mg/l, to be classified as ‘remission’.
Table 1. Demographic details of patients
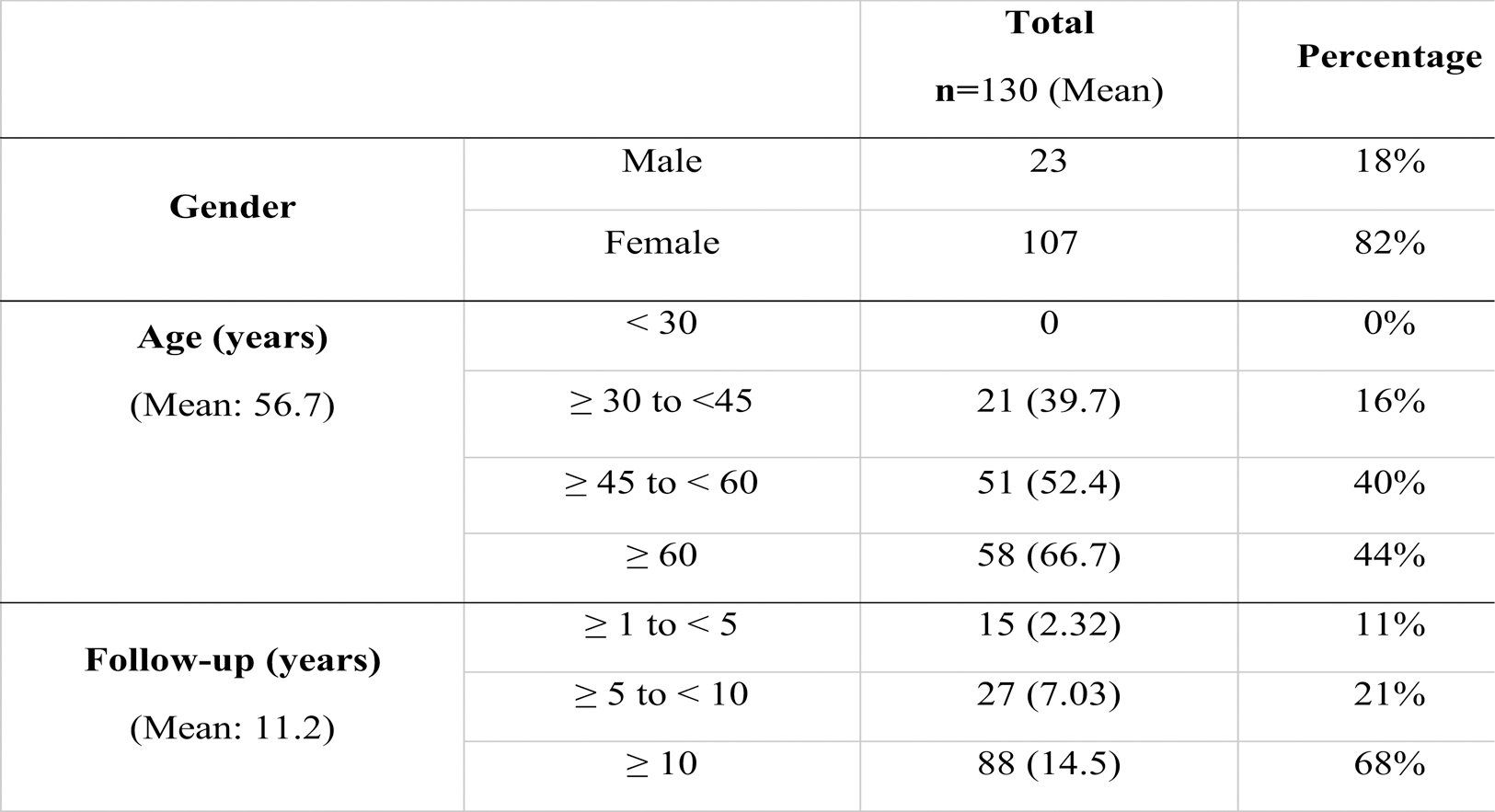
Table 2. LDL-C and hs-CRP blood levels of patients at the last clinic visit.
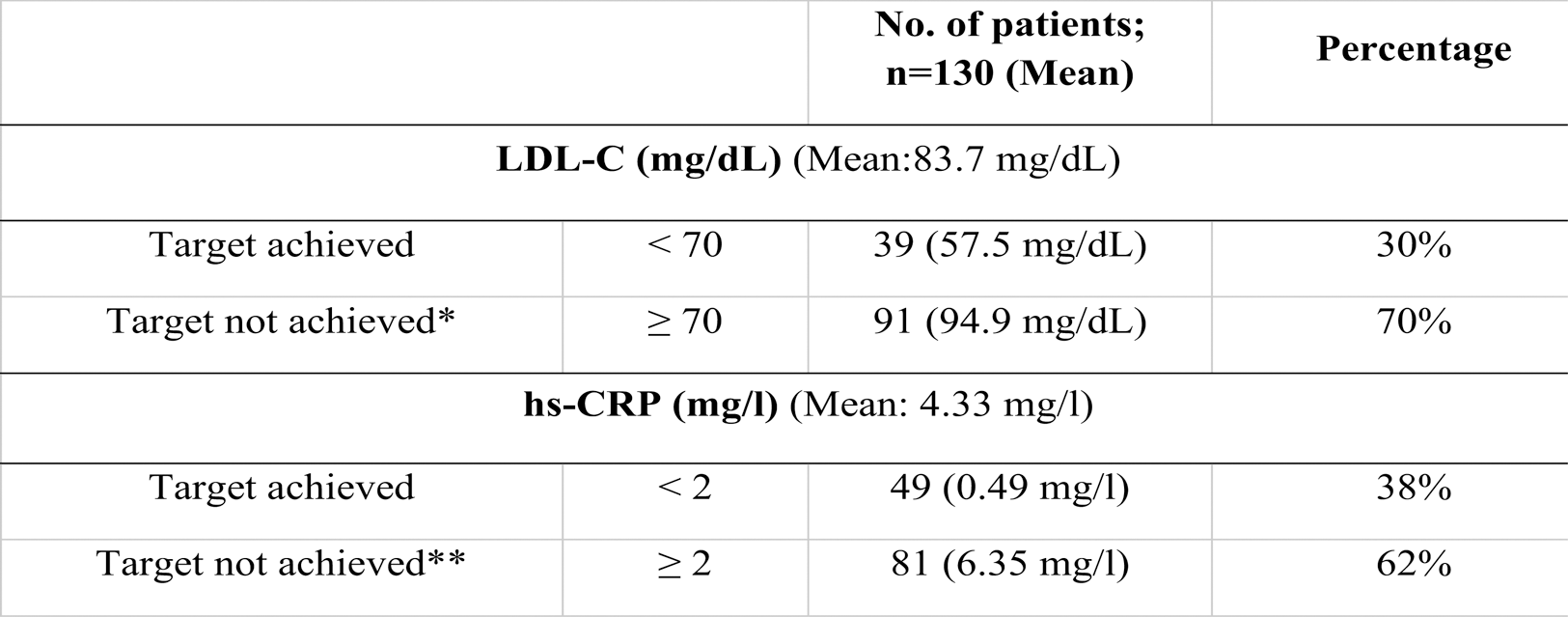
*: Patients having residual cholesterol risk (RCR), **: Patients having residual inflammatory risk (RIR)
REFERENCES: [1] Ridker PM. Residual inflammatory risk: addressing the obverse side of the atherosclerosis prevention coin. Eur Heart J. 2016 Jun 7;37(22):1720-2. doi: 10.1093/eurheartj/ehw024.
[2] Ridker PM. How Common Is Residual Inflammatory Risk? Circ Res. 2017;120:617-9. doi: 10.1161/CIRCRESAHA.116.310527
[3] Drosos GC, Vedder D, Houben E, Boekel L, Atzeni F, Badreh S, et al. EULAR recommendations for cardiovascular risk management in rheumatic and musculoskeletal diseases, including systemic lupus erythematosus and antiphospholipid syndrome Ann Rheum Dis 2022;81:768–779.
Acknowledgements: NIL.
Disclosure of Interests: Anand Malaviya yes, Babita Bondge: None declared