

Background: Juvenile Idiopathic Arthritis (JIA) is a heterogenous group of autoimmune disorders characterised by chronic joint inflammation of unknown aetiology lasting 6+ weeks, with onset before the age of 16. There is currently limited information about long-term outcomes for adults with JIA (including prior classifications and naming), many of whom were diagnosed prior to DMARD and biologic therapies.
Objectives: This collaborative study between three patient organisations investigated the long-term outcomes for adults with JIA in a UK population.
Methods: Adults in the UK aged 18+ who had any diagnosis of a musculoskeletal or rheumatic condition (RMD) were invited to complete an online survey. Respondents provided information about their diagnosis, experiences and attitudes across a range of themes and topics. For inclusion in this analysis, respondents reported a diagnosis of JIA prior to age 16.
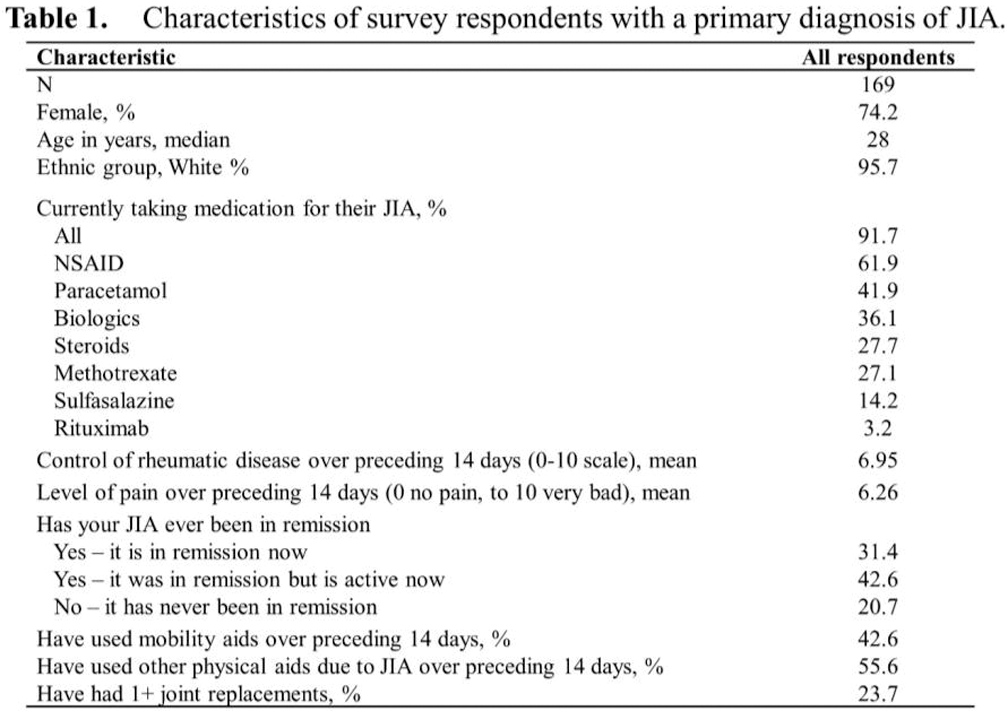
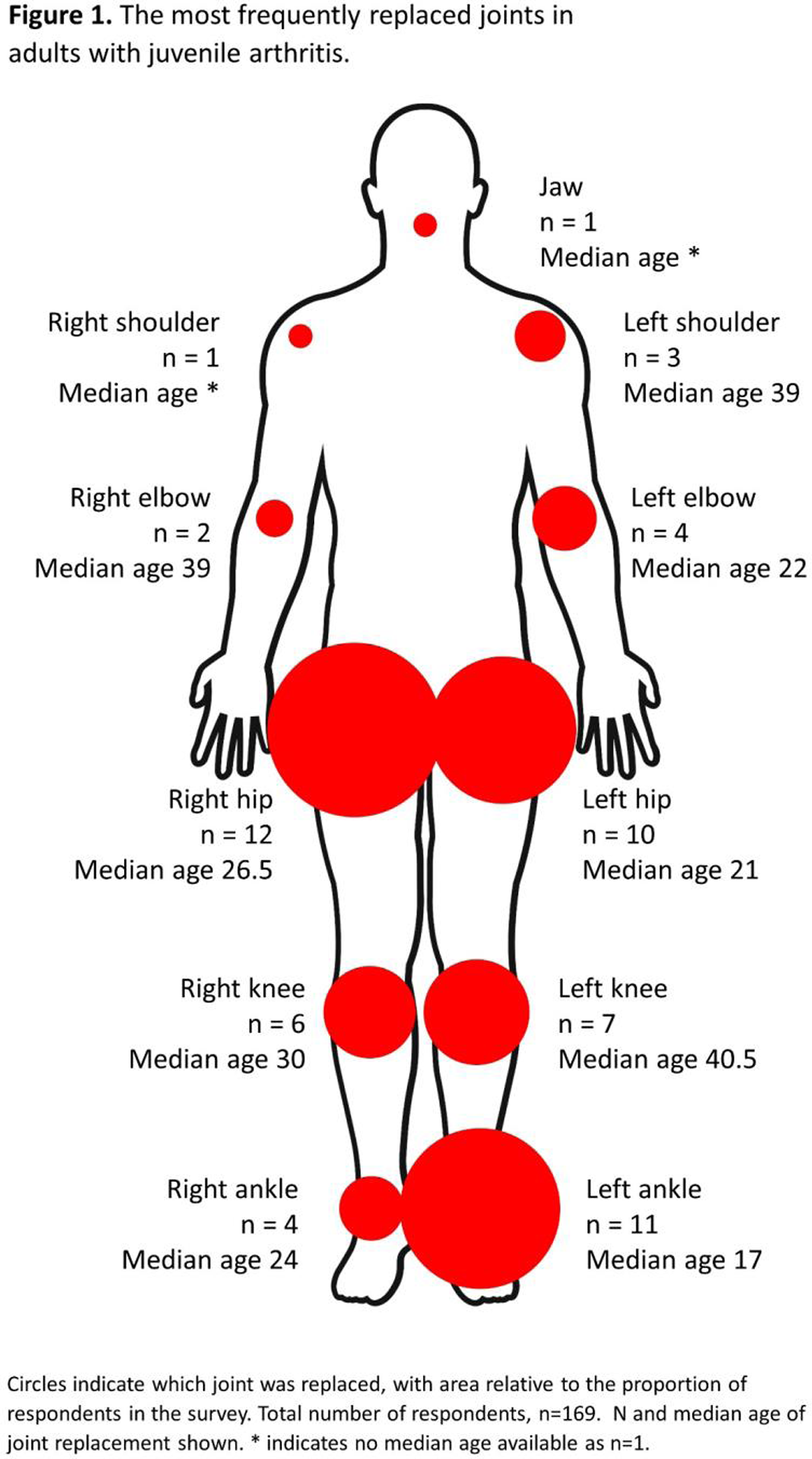
Results: In total, 169 respondents with a primary diagnosis of Juvenile Arthritis completed the survey (Table 1), with 92 (54%) female, and median age 28 years. Of these 92% reported taking medication in the past month due to their JIA (62% took NSAIDs, 36% biologics, 28% steroids, and 27% methotrexate). Respondents mentioned the burden of this: “The pressure of tablets, injections and doctors appointments constantly is mentally draining.” One third (21%) of respondents had never experienced inactive disease, and a further 43% had been in remission but were currently experiencing active disease. Overall, around 64% of respondents were currently experiencing ongoing symptoms due to their JIA. In the two weeks prior to completing the survey, 43% of respondents had used mobility aids due to their JIA, and 56% had used other aids and adaptations because of their condition. The use of aids and adaptations to help physically impacts mental and emotional wellbeing: “Feeling like I was ‘in the way’ with my crutches.” In total, 24% of respondents had received at least one joint replacement (Figure 1), most frequently right hip, left ankle and left hip, with median age of replacement of 26.5, 17.0 and 21.0 years respectively.
Conclusion: Due to potential selection bias, the respondents in this study may be those with some ongoing disease activity or long-term limitation or impact due to their JIA. However, for them, JIA has long-lasting and substantial impacts as they become adults with the disease, with many continuing treatment and experiencing ongoing disease activity. As one respondent reported, “I can’t hold my baby”. Recognizing the impacts and burden of disease for these adults with pediatric-onset conditions is vital in their ongoing care. Whilst children diagnosed with JIA now are considered less likely to have significant long-term physical impacts if adequately, effectively and promptly treated, further research is warranted.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.