

Background: Increasing evidence suggests that body mass index (BMI) may play a causal role in the development of different rheumatic joint disorder [1-3], yet the extent and specificity of this association remains unclear. Mendelian randomization (MR) offers a powerful analytical approach to infer causality by using genetic variants as proxies for an exposure, reducing the impact of confounding and reverse causation common in observational studies [4].
Objectives: This study aimed to systematically review and summarize the evidence from MR studies to appraise the causal role of BMI in a wide range of rheumatic joint disorders.
Methods: A comprehensive literature search was conducted across PubMed, Embase, Web of Science and MEDLINE up to the 17 th of June 2024, to identify MR studies in European populations on genetically predicted BMI and a range of rheumatic joint disorders that included osteoarthritis (OA: hand, hip, knee), rheumatoid arthritis (RA), gout, spondyloarthritis (SpA) and psoriatic arthritis (PsA). Eligible studies were screened and data for study design, population characteristics, genetic instruments, and primary and sensitivity MR analyses were extracted. Using random-effects meta-analysis to account for study heterogeneity, study-specific causal effect estimates from primary and sensitivity MR analyses were combined for overall as well separately for each rheumatic joint disorder. All analyses were conducted using the ‘meta’ package in R v4.4.1.
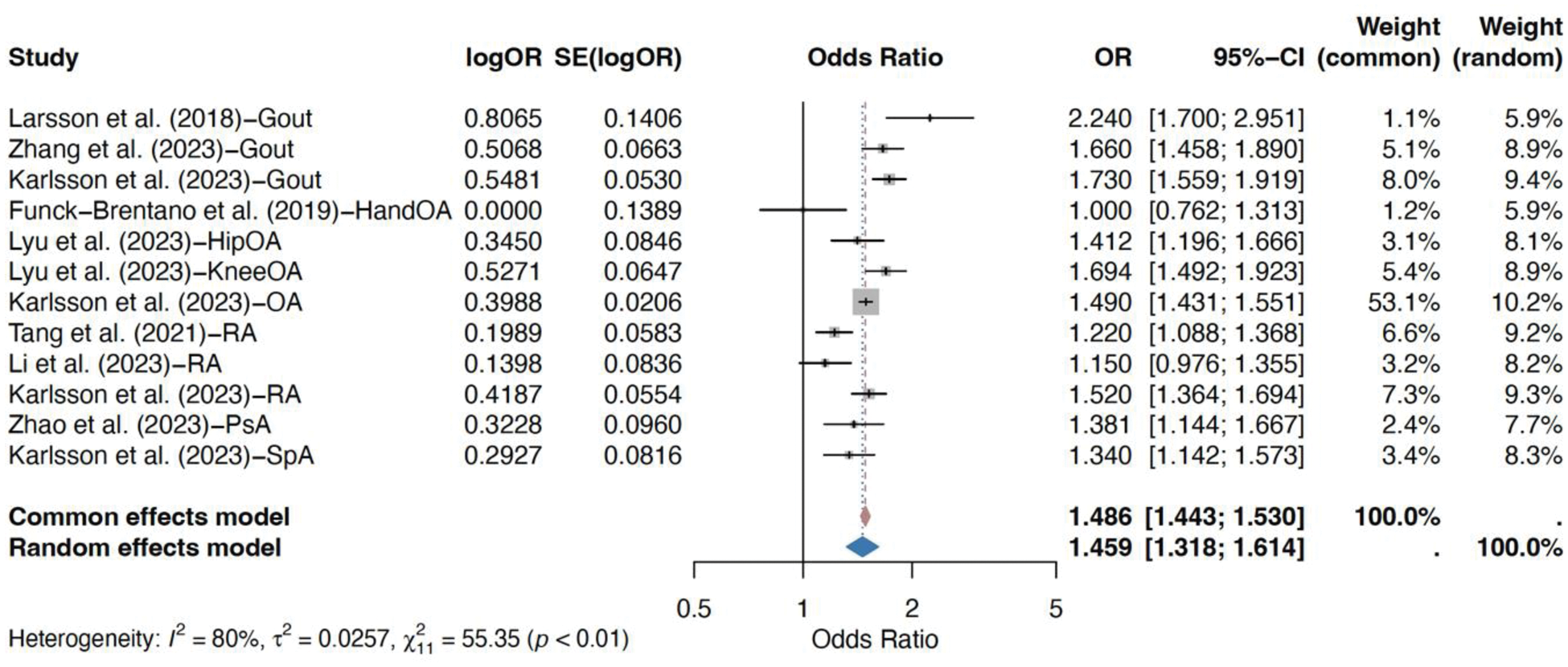
Results: Of 1662 total studies searched in online databases, 24 were included in the systematic review, while the meta-analysis included eight (for 12 outcomes) MR studies. Higher genetically predicted BMI was significantly associated with an increased risk of developing rheumatic joint disorders (inverse-variance weighted OR = 1.45, p < 0.0001) (Figure 1). Consistent results were obtained when the data on sensitivity analyses were summarized in meta-analysis (weighted-median OR = 1.46, p < 0.0001; MR-Egger OR = 1.25, p = 0.004), confirming the robustness of the findings in the primary analysis. Moreover, the causal significance sustained when studies on OA (OR =1.41, p <0.0001), RA (OR = 1.29, p = 0.002), gout (OR = 1.74, p <0.0001), SpA and PsA (OR = 1.35, p <0.0001) were meta-analyzed separately.
Conclusion: This systematic review and meta-analysis provided robust evidence supporting a causal link between elevated BMI and an increased risk of certain rheumatic joint disorders. These findings underscore the clinical importance of BMI and the role of weight management in preventing and potentially alleviating the burden of these disorders. Future MR studies with larger sample sizes and more diverse populations are warranted to further clarify the role of BMI in these and other less studied joint disorders.
REFERENCES: [1] Karlsson T et al. Arthritis & Rheumatology. 2023;75(11):2027-35.
[2] Li X et al. Obesity Facts . 2023;16(6):598-605.
[3] He C et al. European Journal of Human Genetics . 2022;30(5):540-6.
[4] Sekula P et al. Journal of the American Society of Nephrology. 2016;27(11):3253-65.
Forest plot illustrating the meta-analysis results for the association between genetically predicted body mass index (BMI) and risk of rheumatic joint disorders. The estimates were obtained from inverse variance weighted (IVW) analyses conducted in respective studies. Estimates are presented as odds ratios (OR) and their 95% confidence intervals (CIs) for a one standard deviation increase in genetically predicted BMI. OA: osteoarthritis, RA: rheumatoid arthritis, PsA: psoriatic arthritis, SpA: spondyloarthritis.
Acknowledgements: We thank all the participants who contributed in respective GWASs and the authors of Mendelian randomization studies who made the data/summary statistics data available.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (