

Background: Antiphospholipid syndrome (APS) is a systemic disease characterized by thrombotic events and/or pregnancy morbidity in the presence of persistent antiphospholipid antibodies (aPL). This study aimed to describe the clinical and immunological features of a cohort of patients with APS followed at a tertiary center and to find potential predictors for thrombosis.
Objectives: This study aimed to describe the clinical and immunological features of a cohort of APS patients and to identify potential predictors for thrombosis.
Methods: We included all patients diagnosed with APS according to Sydney criteria (2006), followed at a rheumatology tertiary center from January 1996 to December 2024. We also assessed the impact of the updated ACR/EULAR classification criteria (2023) on our cohort.
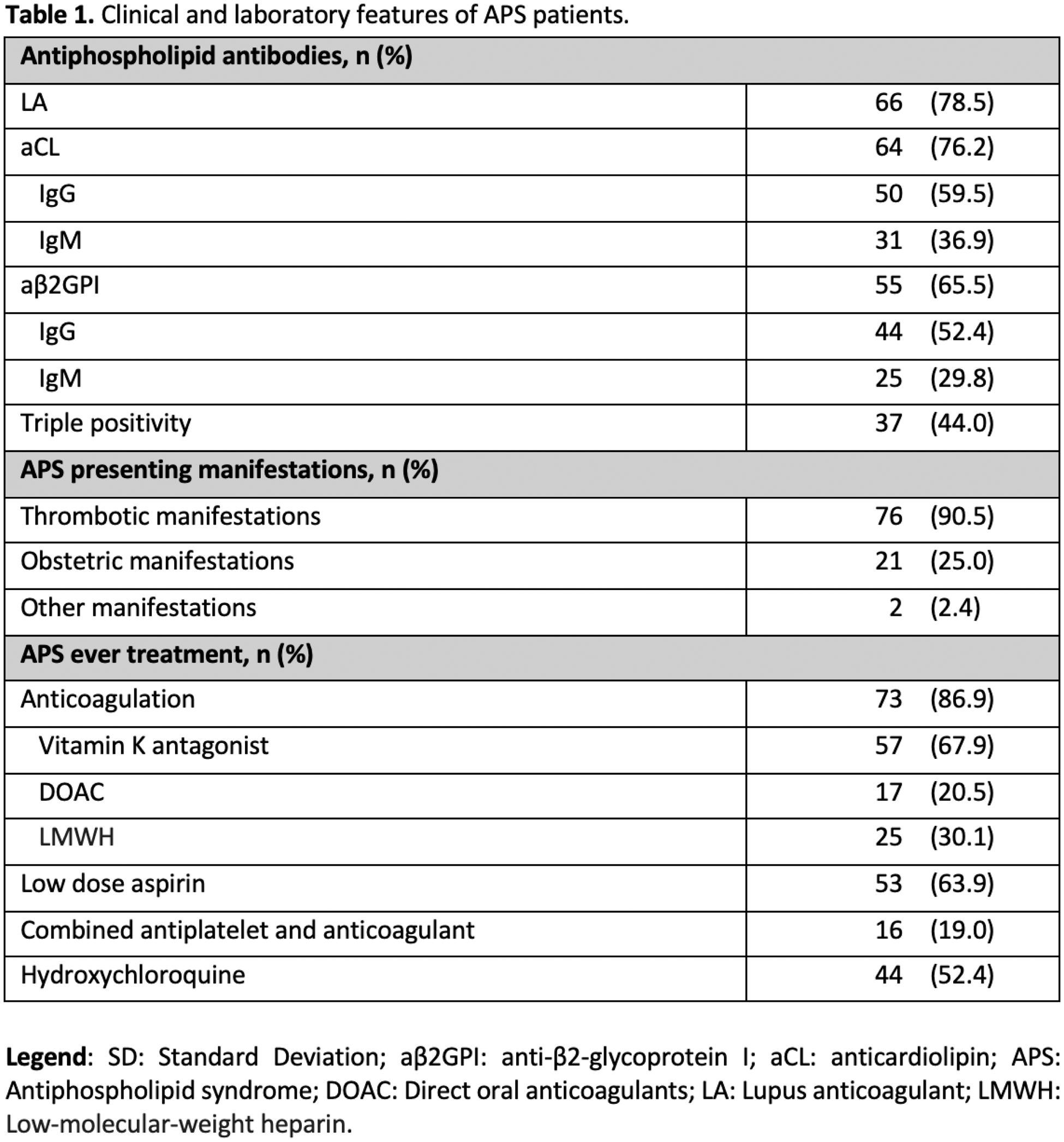
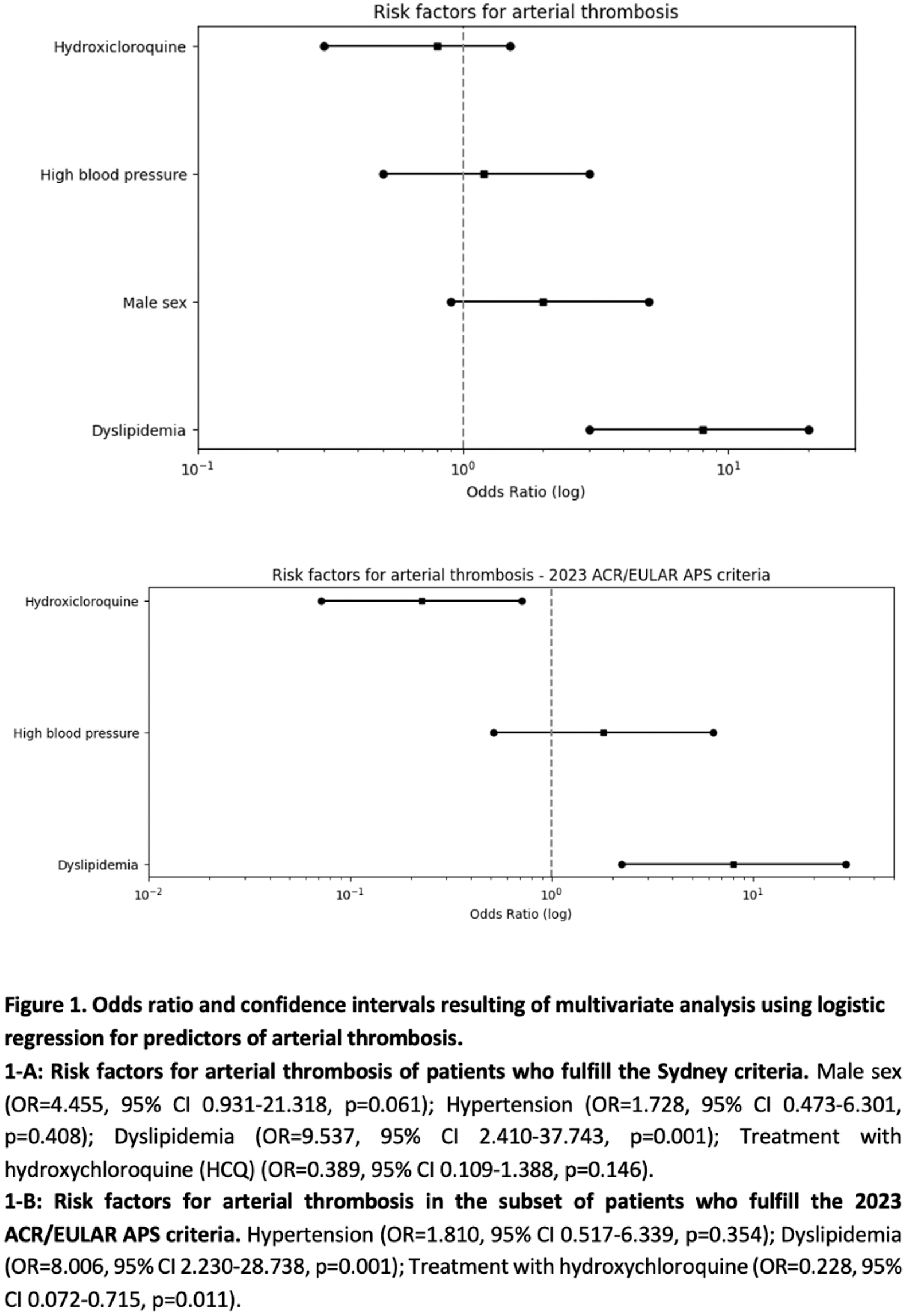
Results: A total of 84 patients fulfilling the Sydney criteria were included, of whom 67 (79.8%) were female and 80 (95.2%) were Caucasian. The mean age at diagnosis was 37.7 ± 14.3 years, and median disease duration was 13.4 ± 9.8 years. Fifty-tree patients had primary APS (63.1%), whereas the remaining (n=31, 36.9%) had secondary APS, most frequently associated with systemic lupus erythematosus (SLE) (n=22/31; 70.9%). Based on the presenting manifestation, 76 patients (90.5%) had thrombotic APS, 46 (54.8%) and 28 (33.3%) of whom with venous or arterial events, respectively. Lower deep vein thrombosis (40.5%), pulmonary embolism (20.2%) and stroke (16.7%) were the most frequent. Obstetric morbidity was the first disease manifestation in 21 patients (25.0%) and two patients (2.4%) were diagnosed due to Sydney non-criteria manifestations – Libman–Sacks endocarditis. Over a follow-up of 28 years, one patient (1.2%) died from non-APS related causes. When applying the 2023 updated ACR/EULAR criteria, only 59/84 patients (70.2%) reached the composite score of the new criteria. Therefore, the diagnosis of thrombotic APS in our cohort decreased from 76 to 63 due to high cardiovascular risk in 6 cases, high risk for thromboembolism in 5 patients, and IgM aPL profile in 2 cases. Patients with obstetric morbidity decreased from 21 (25.0%) to 9 (15.3%). Cardiovascular (CV) comorbidities were common, with smoking (48.8%), hypertension (42.9%), and dyslipidemia (42.9%) being the most frequent risk factors followed by obesity (29.8%) and diabetes (7.1%). Regarding antibody profile, lupus anticoagulant was present in 66 patients (78.5%), IgM/IgG anticardiolipin in 64 patients (76.2%) and IgM/IgG anti-β2-glycoprotein I antibodies were detected in 55 patients (65.5%). Thirty-seven patients (44.0%) showed triple antibody positivity. Anticoagulation was used in 73 patients (86.9%), most often with vitamin K antagonists (VKA) in 57 patients (67.9%); low-dose aspirin (LDA) was used in 53 patients (63.9%) and combined antiplatelet/anticoagulant therapy in 16 patients (19.0%). Hydroxychloroquine (HCQ) was prescribed to 44 patients (52.4%) - 32/84 (38.1%) had an inflammatory rheumatic disease, of which 22/84 (26.2%) was SLE. Bleeding events (according to the definitions of the ISTH) occurred in 10 patients (13.9%). Of these, 7 (70%) had major hemorrhagic events and 3 (30%) were under combined antiplatelet/anticoagulant therapy. Thrombotic recurrence was noted in 13 patients (15.5%) - 8 (61.5%) venous and 5 (38.5%) arterial events. In univariate analysis we found arterial thrombosis to be more frequent in men (64.7% vs 25.4%, p<0.002, OR=5.39; 95% CI [1.73; 16.81]) and in patients with CV comorbidities, such as hypertension (52.8% vs 18.8%, p=0.001; OR 4.84; 95% CI [1.82;12.86]) and dyslipidemia (12.5% vs 61.1%, p<0.001 OR 11.00, 95% CI [3.71;32.61]), and less frequent in patients treated with HCQ (18.2% vs 50%, p=0.002 OR 4.50; 95% CI of [1.69; 12.05]). No associations were found with venous thrombosis. Recurrence of thrombotic events was more frequent in patients with dyslipidemia (25.0% vs 8.3%, p=0.037; OR 3.67; 95% CI [1.03; 13.08]). Similar results were obtained when analyzing the subset of patients who only fulfill the updated classification criteria. In multivariate analysis, considering the full cohort of patients, dyslipidemia was associated with arterial thrombosis and thrombotic recurrence. We found no risk factors for venous thrombosis. When performing multivariate analysis in the subgroup of patients fulfilling the new classification criteria, HCQ seemed to be protective of arterial thrombosis (Figure 1).
Conclusion: In APS patients, arterial thrombosis and the risk of thrombotic recurrence were linked to CV comorbidities, namely dyslipidemia, highlighting the need for tight control of these comorbidities. HCQ exhibited a trend to be protective for arterial thrombosis, namely in those patients fulfilling the new and more specific updated classification criteria.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (