

Background: Systemic sclerosis (SSc) is a rare autoimmune disease with high morbidity and mortality. Vasculopathy is central in its pathophysiology, potentially coinciding with deranged vascular repair. Angiogenic T-cells (Tang) are a recently identified subgroup of T-cells, that have been shown to affect their function through tissue migration and vascular repair. These cells have been indicated to play a role in a number of diseases involving vascular components. Tang cells have been linked to vasculogenesis and endothelial repair, and their levels have been associated with microvascular damage in SSc. Notably, Tang proportions have been shown to decrease in autoimmune-disease-associated interstitial lung disease (ILD) when compared to healthy controls [1]. However, their specific role in the pathophysiology of SSc is unclear. This study explores the association between Tang cells, and SSc-ILD – the leading cause of mortality in SSc, along with related patient characteristics.
Objectives: We hypothesize that, in SSc-ILD, Tang cells migrate to sites of vascular injury in the lungs, resulting in a decrease peripheral blood Tang proportion. We aim to explore this hypothesis by identifying the relationship between Tang proportions and SSc-ILD presence, as well as severity as measured by lung function tests. Additionally, we aim to identify the relationship between Tang proportions and other relevant patient characteristics, and peripheral vasculopathy as measured by capillary microscopy.
Methods: This study included 83 SSc patients and 23 healthy controls (HC). Patient subgroups based on SSc subtypes and manifestations were identified, and patient characteristics were recorded. Tang cells (defined as CD3+, CD31+, CXCR4+) were identified and analyzed on flow cytometry in previously stored peripheral blood mononuclear cells (PBMCs). These were further subdivided into CD4+, CD8+, and total subgroups. Additionally, patients were subdivided into groups based on capillary microscopy results (early, active, late SSc; normal; non-specific), which were used to assess peripheral vasculopathy. Lung function tests were used to assess ILD severity. Lastly, angiogenic cytokines interleukin-8 (IL-8) and vascular endothelial growth factor (VEGF) levels were measured in patient serum samples. Tang proportions were then compared between the studied patient subgroups and healthy control groups and tested for association with the relevant recorded clinical characteristics.
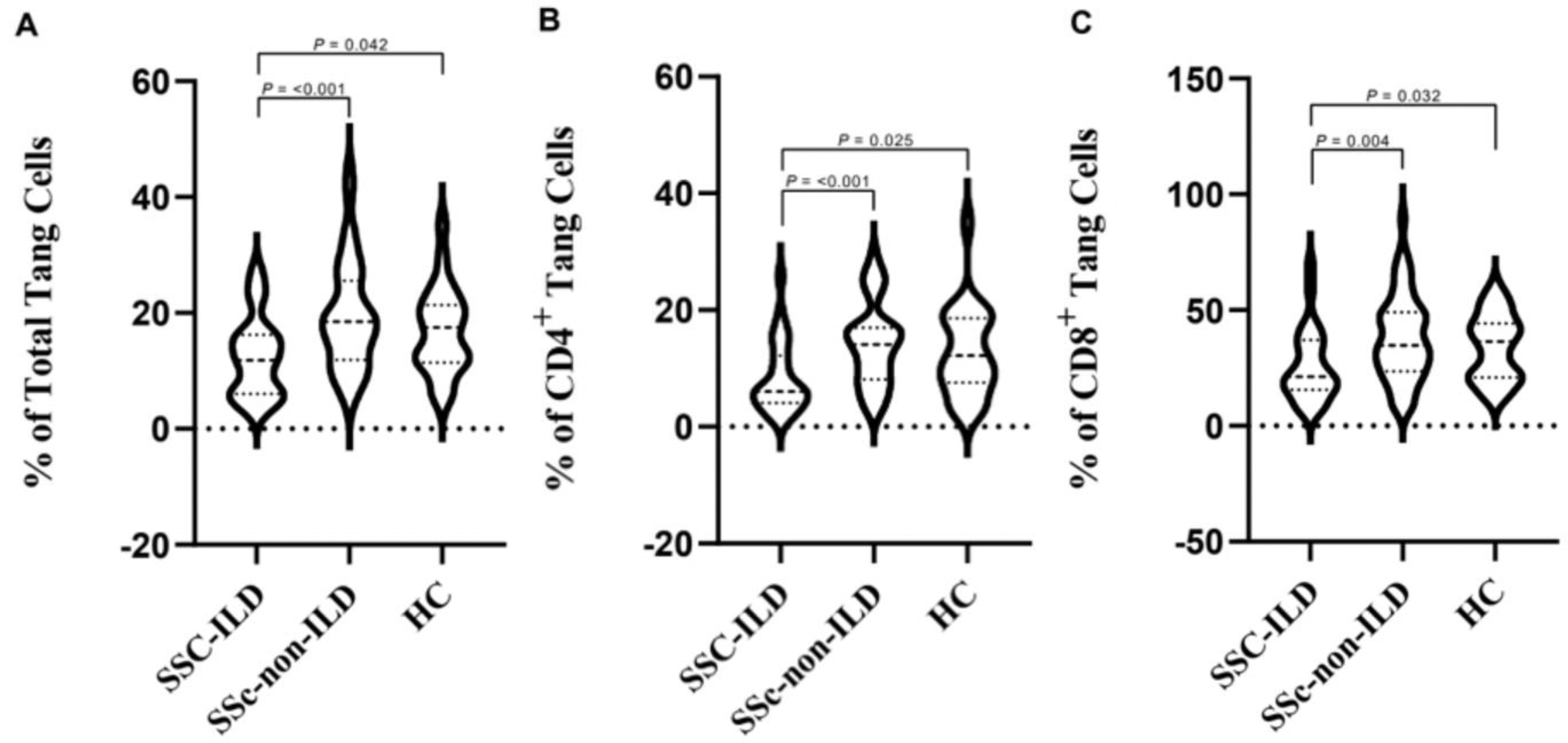
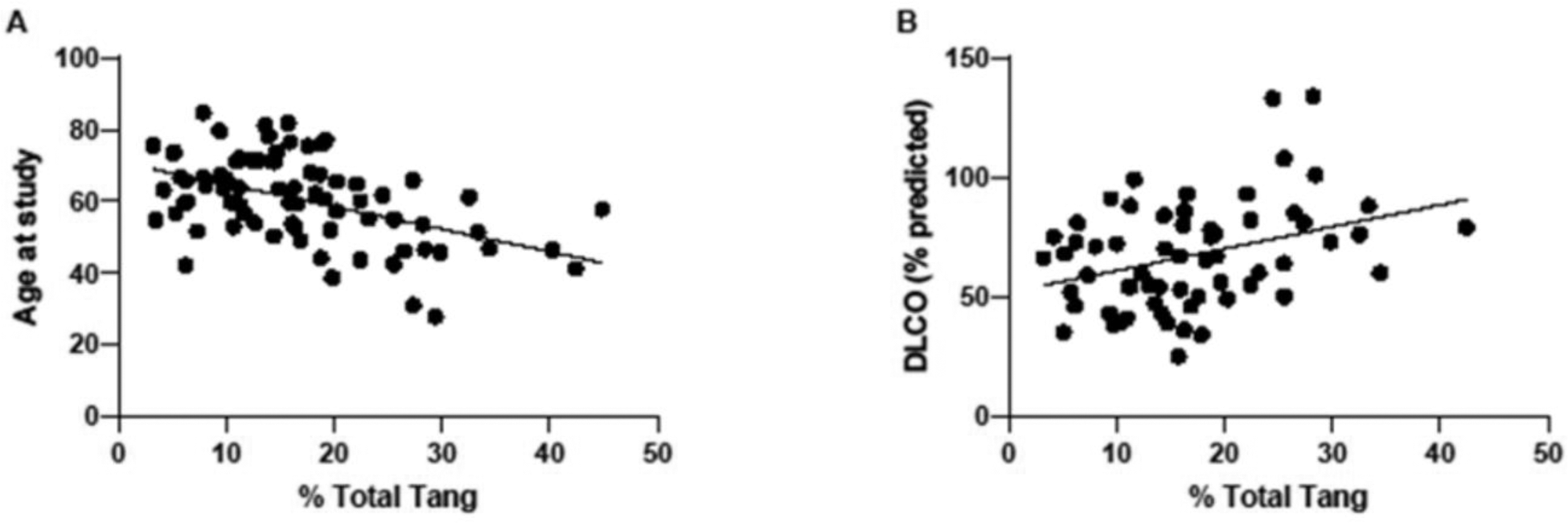
Results: As a whole, the SSc group did not differ significantly from the control group, regarding Tang proportions. The median proportion of total Tang cells was 11.8% (IQR = 6.05-16.25) in SSc-ILD, 18,5% (IQR = 11.90-25.55) in SSc-non-ILD, and 17.5% (IQR = 11.40-21.34) in HC. Patients with SSc-ILD had significantly lower peripheral blood total, CD4+, and CD8+ Tang proportions, when compared to patients without SSc-ILD (p = <0.001) as well as HC (p = 0.042). Patients without SSc-ILD did not differ significantly from HC. Additionally, Tang cells correlate positively with the diffusion capacity of the lung (DLCO) (total Tang, p = 0.007; CD4+ Tang, p = 0.021). Interestingly, patients classified as having an early scleroderma vasculopathy pattern on capillary microscopy had significantly higher total Tang proportions than those classified as active and late (0.046). Lastly, proportions of all Tang subgroups correlated inversely with age (p = <0.001). No difference in age was observed between the studied subgroups.
Conclusion: Patients with SSc-ILD had significantly lower total, CD4+, and CD8+ Tang proportions when compared to both SSc-non-ILD patients and HC. Additionally, Tang cells correlated positively with DLCO and were associated with specific vasculopathy patterns, further alluding to a possible involvement of Tang cells in vascular repair in ILD. Future studies should focus on elucidating the fate of these cells in SSc-ILD, possibly by looking at migration axes such as the SDF-1/CXCR4 axis, and their role as potential therapeutic targets.
REFERENCES: [1] Verónica Pulito-Cueto, Remuzgo-Martínez S, Genre F, Belén Atienza-Mateo, Mora-Cuesta VM, Iturbe-Fernández D, et al. Angiogenic T Cells: Potential Biomarkers for the Early Diagnosis of Interstitial Lung Disease in Autoimmune Diseases? Biomedicines. 2022 Apr 5;10(4):851–1.
Violin plots showing the differences in proportions of Tang cells expressed as % of total Tang-cells (A), CD4+ (B), and CD8+ (C) Tang-cells across three groups (SSc-ILD, SSc-non-ILD, HC). P-values are displayed for significantly different groups.
Scatter plots showcasing significant correlations between percentages of total Tang cells and select variables. (A) The percentage of total Tang significantly (p = <0.001) and negatively (ρ = -0.460) correlates with patient age at the time of study. No significant differences in age were observed between the studied groups. (B) The percentage of total Tang significantly (p = 0.007) and positively (ρ = 0.336) correlates with DLCO (% predicted). DLCO abnormalities are known early markers of ILD.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (