

Background: Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by the presence of antiphospholipid antibodies (aPLs) and clinical manifestations such as vascular thrombosis and pregnancy complications. Among the various aPL targets, βeta 2 Glycoprotein 1 (β2GPI) and its Domain I (DI) have emerged as significant antigens. Recent research highlights the role of IgA subclasses, IgA1 and IgA2, in APS, suggesting that their preferential binding patterns could have clinical implications.
Objectives: To investigate the antigen specificity and clinical significance of IgA subclasses (IgA1 and IgA2) in antiphospholipid syndrome (APS) patients.
Methods: Serum samples were collected and processed from 102 APS patients and 7 healthy controls (HC). Among these, 42 APS patients were identified as positive for both serum IgA anti-β2GPI (aβ2GPI) and anti-DI (aDI) using enzyme-linked immunosorbent assay (ELISA), with positivity determined based on a cut-off calculated as the mean +3 standard deviations of HC values. Fisher’s exact test was applied to identify clinical associations without implying causality. We analysed several antibodies, including IgA1 and IgA2 anti-D1, IgA1 and IgA2 anti-β2glycoprotein (β2GP), lupus anticoagulants (LA), and the presence or absence of combinations of three criteria antibodies (LA, IgG anti-cardiolipins, and IgG anti-β2GP). These combinations were categorised into four groups: none present, one present, two present, and all three present. In addition, vascular risk factors such as hypertension, smoking, and hyperlipidaemia were included in the analysis. To identify variables significantly associated with complications such as pregnancy-related complications and thrombosis, we used the Boruta algorithm, a feature selection method within the random forest (RF) model. After identifying the important variables, we fitted them into a penalized LASSO regression model to calculate odds ratios (ORs). P-values were subsequently derived using conventional multivariate logistic regression.
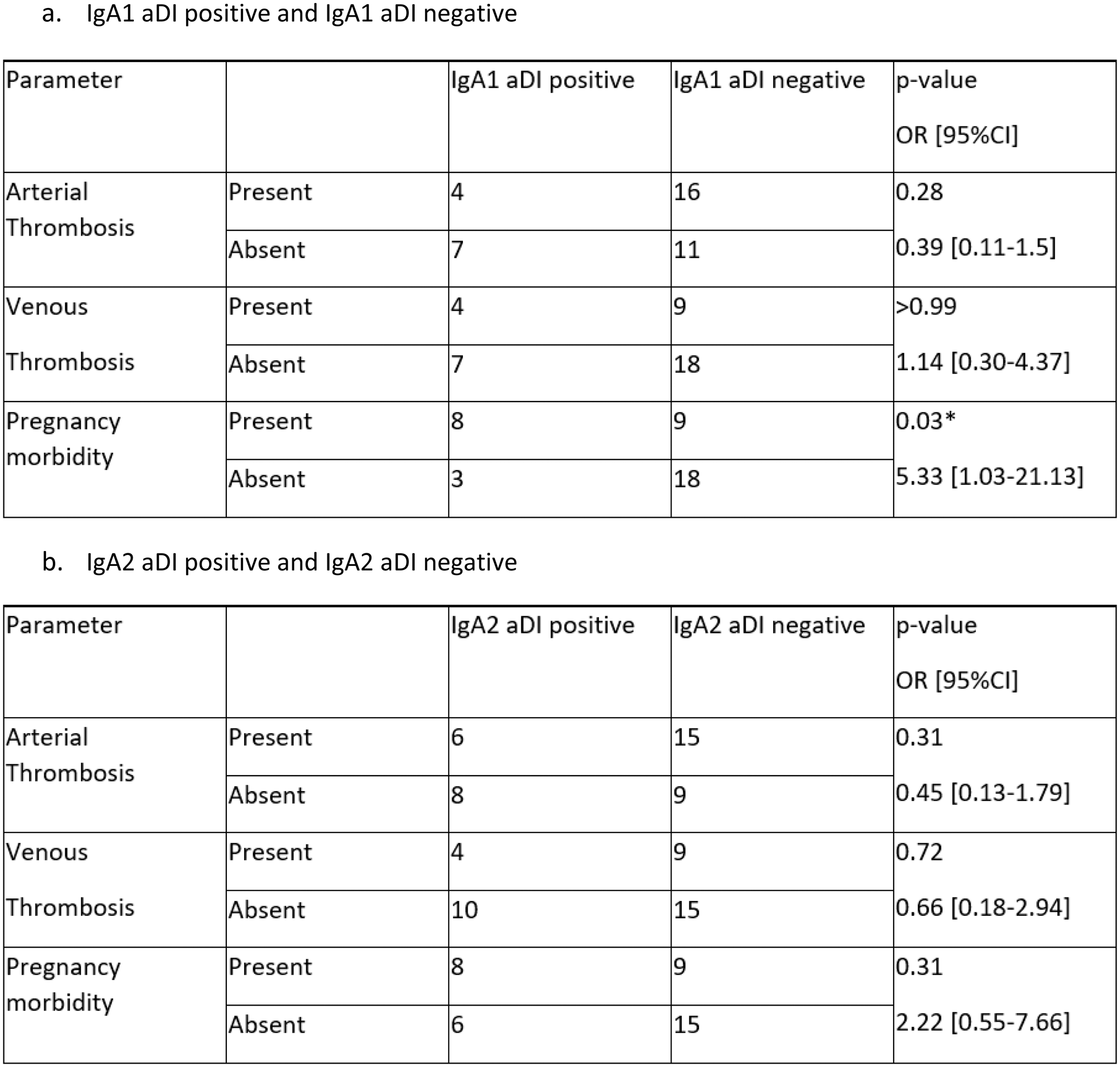
Results: Figure 1. A results show that the IgA1 level was higher for DI compared to β2GPI, whereas the IgA2 level was higher for β2GPI compared to DI, suggesting a preferential binding of IgA1 to DI (a protein antigen) and IgA2 to β2GPI (a glycoprotein). Of interest, Figure 1 B showed that there is indeed a greater proportion positive for IgA2 β2GPI. A significant relationship found between IgA1 aDI positivity and pregnancy morbidity (p=0.03) (Figure 1 C) where the odds of pregnancy morbidity were 5.33 times higher in IgA1 aDI positive patients compared to IgA1 aDI negative patients. IgA1 aD1 emerged as the only significant positive predictor of pregnancy-related complications (Figure 2 A-B), compared to other groups (e.g., thrombosis or no complications; note that only four patients had no complications). This antibody was associated with more than a fivefold increased risk of pregnancy-related complications, with an adjusted p-value of 0.0228 and an adjusted AUROC of 0.84 (95% CI: 0.73–0.91). These findings suggest that traditional vascular risk factors, such as hypertension and smoking, were strongly associated with thrombosis (Figure 2 C-D). LA also emerged as an independent risk factor for thrombosis. Interestingly, vascular risk factors such as smoking, hypertension, and hyperlipidemia were identified as important risk factors for arterial thrombosis (Figure 2 E) but not for venous thrombosis, where no variables stood out as significant in the RF model (data not shown).
Conclusion: This study highlights the distinct roles of IgA subclasses in antiphospholipid syndrome (APS), demonstrating their preferential binding patterns to specific antigens and clinical relevance. IgA1 showed a stronger affinity for DI, while IgA2 preferentially targeted β2GPI. Notably, IgA1 aDI emerged as a significant predictor of pregnancy-related complications, emphasizing its potential as a biomarker for risk stratification. These findings advance our understanding of APS pathogenesis and underscore the value of IgA subclasses in enhancing diagnostic accuracy, risk assessment, and developing targeted therapeutic strategies.
(A-C): The preferential binding of the antibody against the antigen . A. Comparison of medians: (a) IgA1 aβ2GPI vs (b) IgA2 aβ2GPI and (c) IgA1 aDI vs (d) IgA2 aDI. The dotted line represents the cut-off value (+3SD of HC). B. More glycoprotein binding affinity: (a) Venn diagram and (b) Upset plot both show the APS patients unique for IgA2 β2GPI. C. Highlights a significant association between IgA1 aDI positivity and pregnancy morbidity (p=0.03), with IgA1 aDI positive patients having 5.33 times higher odds of pregnancy morbidity compared to IgA1 aDI negative patients.
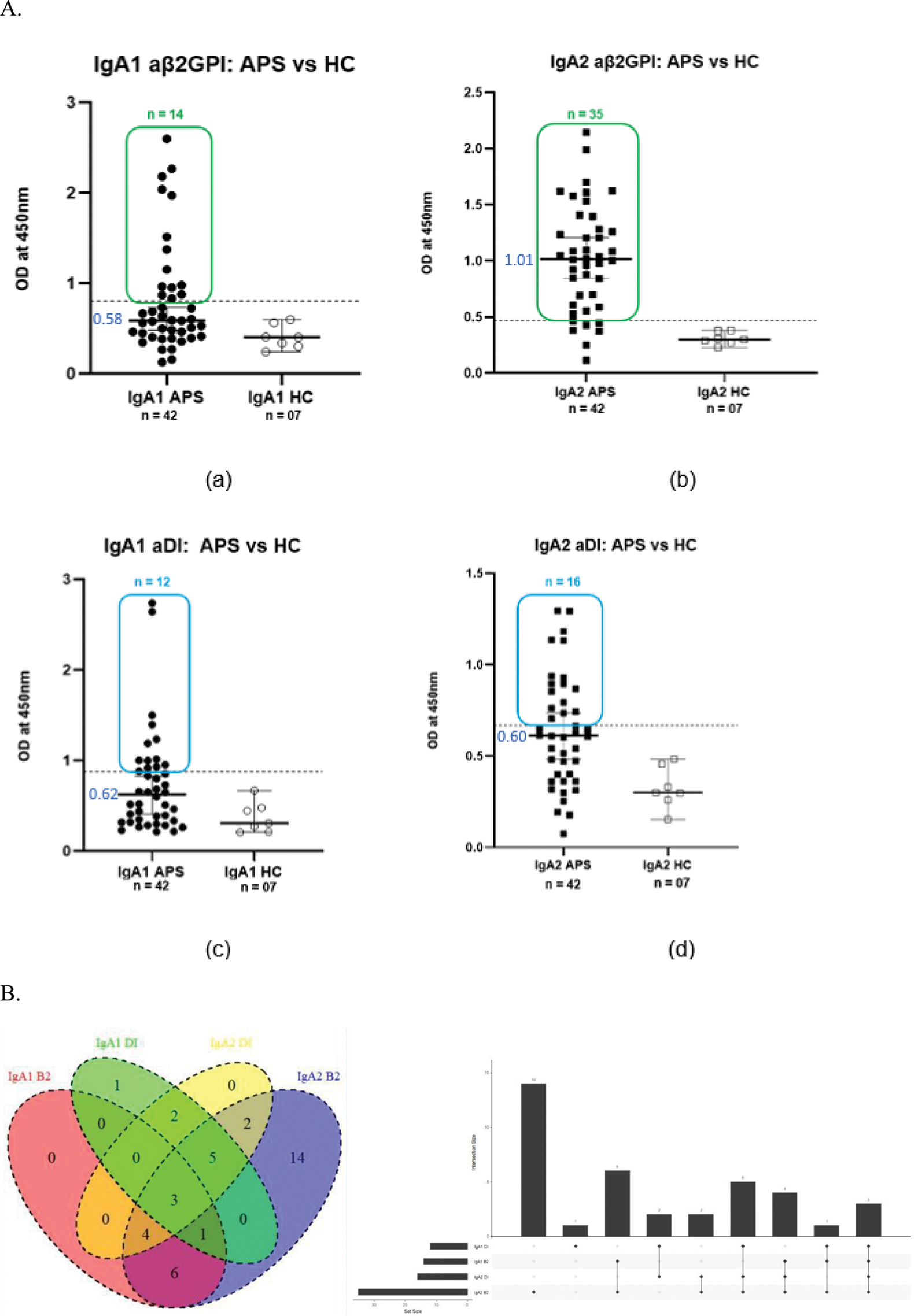
Total number of individuals n = 38† out of 42.†4 individuals’ clinical data were unknown. *p=0.05 significant.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (