

Background: Rheumatoid arthritis (RA) is a chronic autoimmune disease, characterised by cross-reactive anti-modified protein antibodies (AMPA). These include anti-citrullinated (ACPA), anti-carbamylated (ACarP) and anti-acetylated (AAPA) protein antibodies. While these autoantibodies are typically found only in RA patients, AAPA IgM forms a striking exception, being present in healthy individuals as well [1]. We hypothesise that AAPA IgM may be part of a healthy normal immune response and constitute a starting point for antibody maturation potentially leading to emergence of other AMPAs.
Objectives: To evaluate the serological profile of AAPA IgM across different stages of health and disease.
Methods: Using in-house AMPA ELISAs, we measured AAPA IgM and other AMPA in various cohorts. This analysis encompassed cord blood serum samples, pre-symptomatic individuals (pre-RA cohort) with serum collected before and after symptom onset and established RA patients from the Early Arthritis Clinic (EAC) with longitudinal sera spanning up to five years. Cord blood was analysed as only IgG antibodies are transported across the placenta and therefore the presence of IgM would suggest foetal origin; a natural antibody feature.
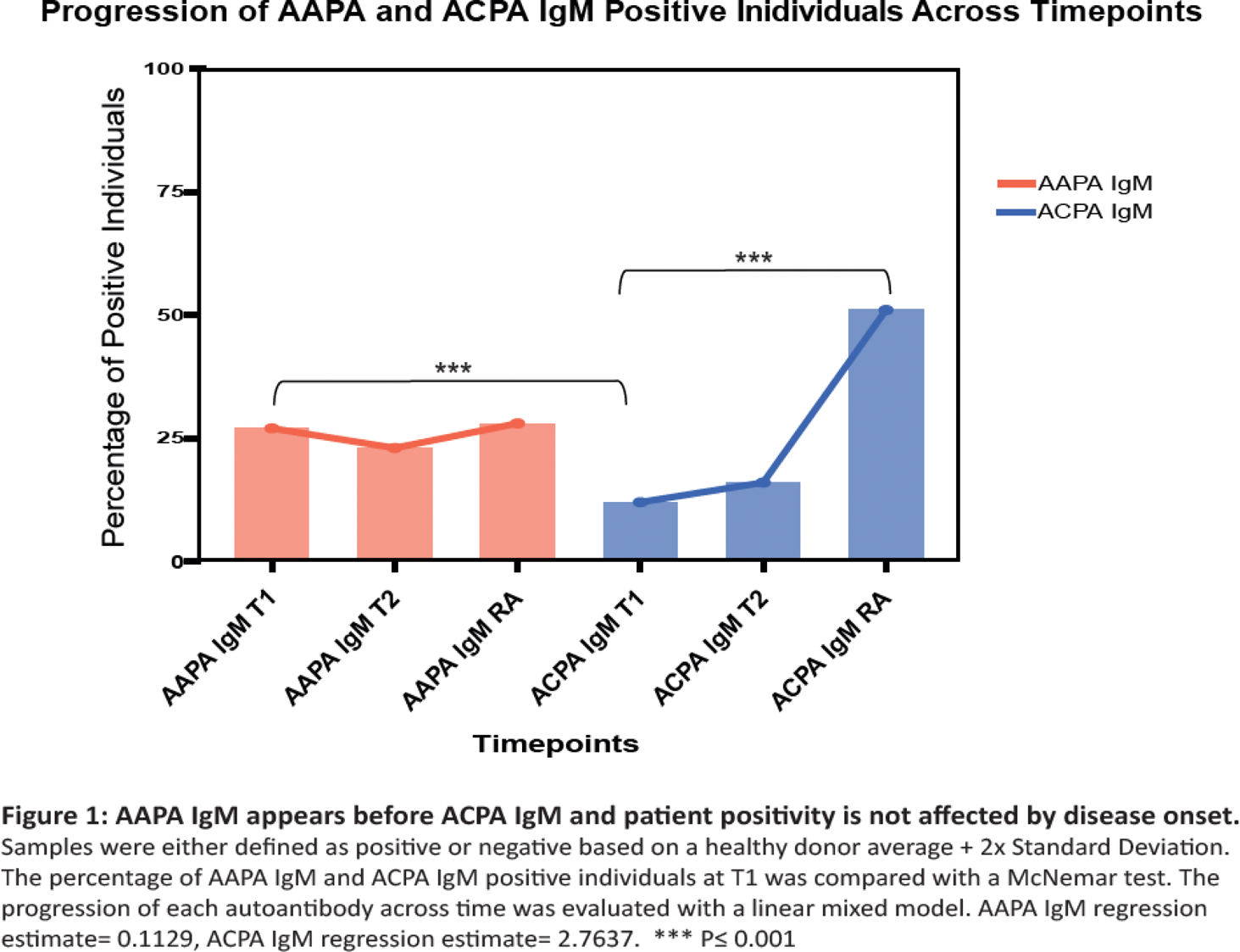
Results: Our investigation did not detect AAPA IgM in cord blood. In the pre-RA cohort, we found significantly more samples positive for AAPA IgM at the earliest, asymptomatic stage (27.3%) compared to ACPA IgM (11.7%). Upon disease onset anti-citrullinated peptide reactivity increased, with ACPA IgM positivity becoming 51.2%. Unlike ACPA IgM, the AAPA IgM response remained stable over time with 27.9% positive patients at symptom onset (Figure 1). It appears that AAPA IgM is not required for AMPA responses to develop, since 67.9% of patients negative for AAPA IgM at the earliest timepoint, went on to produce other AMPAs over time. Likewise, our longitudinal EAC analysis demonstrated that AAPA IgM levels remained stable even after RA onset.
Conclusion: We did not obtain evidence suggesting that AAPA IgM are found at birth, possibly due to the extremely low/absence of total IgM found in newborns. Even though AAPA IgM emerge before other AMPAs, no association between AAPA IgM positivity and RA onset or AMPA maturation was evident, indicating that it is unlikely that AAPA IgM serves as the sole origin of matured AMPA responses in RA. Based on the stable serological profile of AAPA IgM, our data supports the notion that it is part of a normal immune response commonly found in individuals without having any adverse health effects, as it does not appear to be affected by disease onset. Together, our findings provide a better insight on the dynamics of the AMPA responses. Better understanding of when AAPA IgM first appears in the immune response, could enable the identification of potential antigen triggers, or reveal clues about early immunological events in RA. Furthermore, understanding the timeline and conditions under which the AMPA response matures could inform the optimal timing for therapeutic intervention, targeting this response before it becomes pathogenic.
REFERENCES: [1] van Wesemael, T. J., Reijm, S., Kawakami, A., Dorjée, A. L., Stoeken, G., Maeda, T., Kawashiri, S. Y., Huizinga, T. W. J., Tamai, M., Toes, R. E. M., & van der Woude, D. (2024). IgM antibodies against acetylated proteins as a possible starting point of the anti-modified protein antibody response in rheumatoid arthritis.
Annals of the rheumatic diseases
, 83(2), 267–270.
Acknowledgements: The research received funding through a Vidi-grant of the Dutch Research Council (NWO) (Project Nr 09150172110053 to DvdW).
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (