

Background: Lupus nephritis (LN), a severe complication of systemic lupus erythematosus (SLE), significantly contributes to increased morbidity and mortality among affected patients [1]. Despite advances in treatment, LN remains challenging to manage due to its complex pathogenesis and the lack of reliable biomarkers for monitoring therapeutic response [2]. Previous studies have demonstrated that an interferon-driven plasma cell signature in peripheral blood correlates with active LN, highlighting the critical role of interferon pathways in disease activity [3]. Building on this knowledge, the current study evaluates how interferon-related gene expression and immune cell proportions in peripheral blood respond to LN treatment. Specifically, it focuses on patients treated with interferon α kinoid (IFN-K), a therapeutic vaccine designed to neutralize interferon α subtypes, which has shown potential to reduce disease manifestations in SLE [4]. This analysis aims to provide further insights into the immunological and transcriptomic changes associated with LN treatment.
Objectives: This study aimed to evaluate the changes in interferon-related gene expression and immune cell proportions in peripheral blood over time in response to lupus nephritis (LN) treatment with interferon α kinoid (IFN-K), and to assess their association with disease activity.
Methods: Dataset GSE72747 was downloaded from the Gene Expression Omnibus platform. This dataset contains transcriptomic dataset of patients with LN treated with interferon α kinoid (IFN-K), a therapeutic vaccine consisting of inactivated IFN α2b coupled to a carrier protein. It was observed that, when injected, induces a polyclonal antibody response that neutralized all IFNα subtypes, preventing disease manifestations. Mean fluorescence intensity (MFI) values of patients at 0m, 3m, and 6m after the injection for the genes IFI27, IFI44, IFI44L, RSAD2, MX1, OAS3, and ISG15 were retrieved. CibersortX was utilized to assess the percentages of 22 different types of immune cells, and a 2-way ANOVA test was performed to identify differences between the genes’ MFIs and the proportions of immune cells. The same test was utilized to identify changes in Disease Activity Index Disease Scores (SLEDAI) in time. Statistical significance was set as p < 0.05.
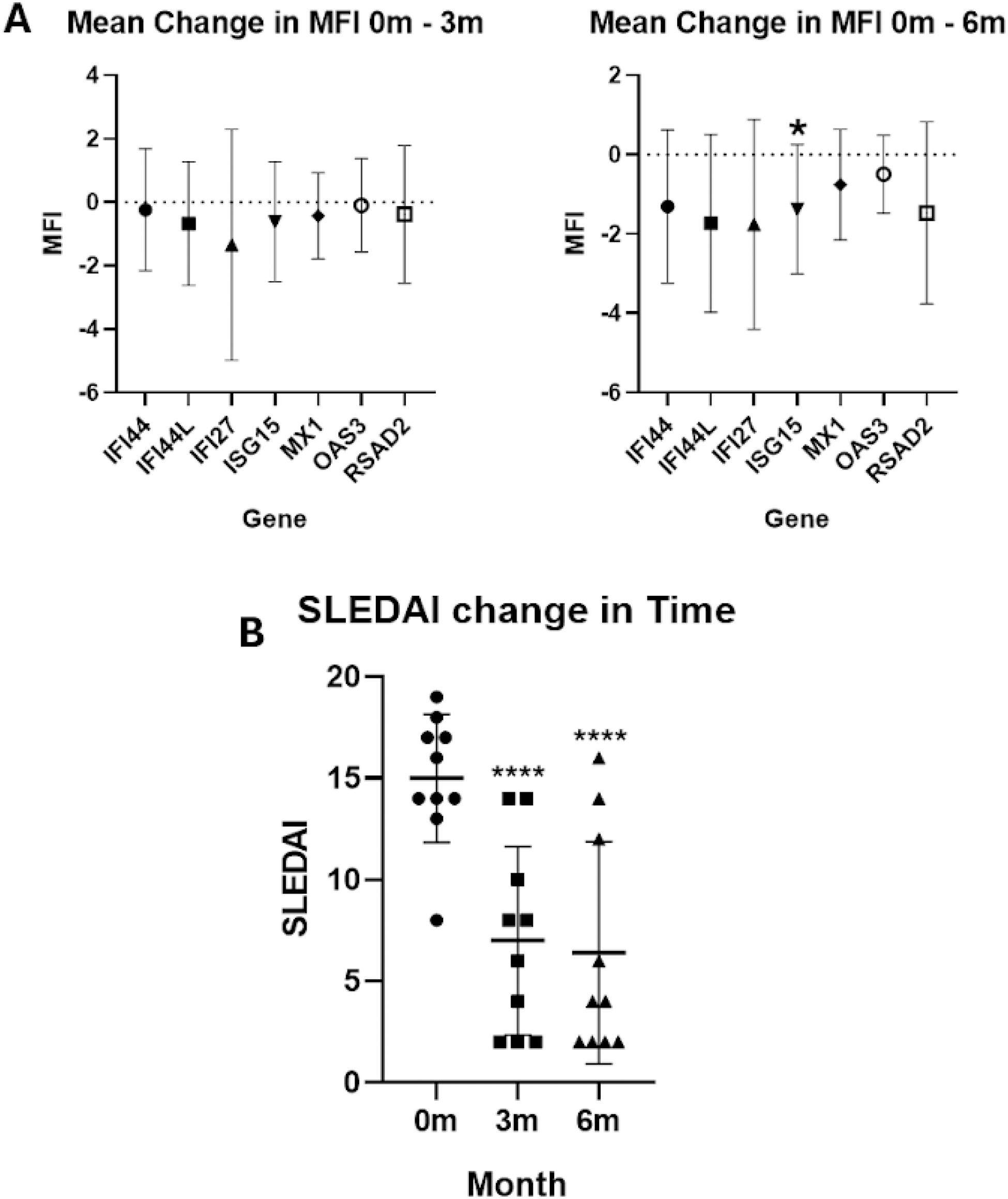
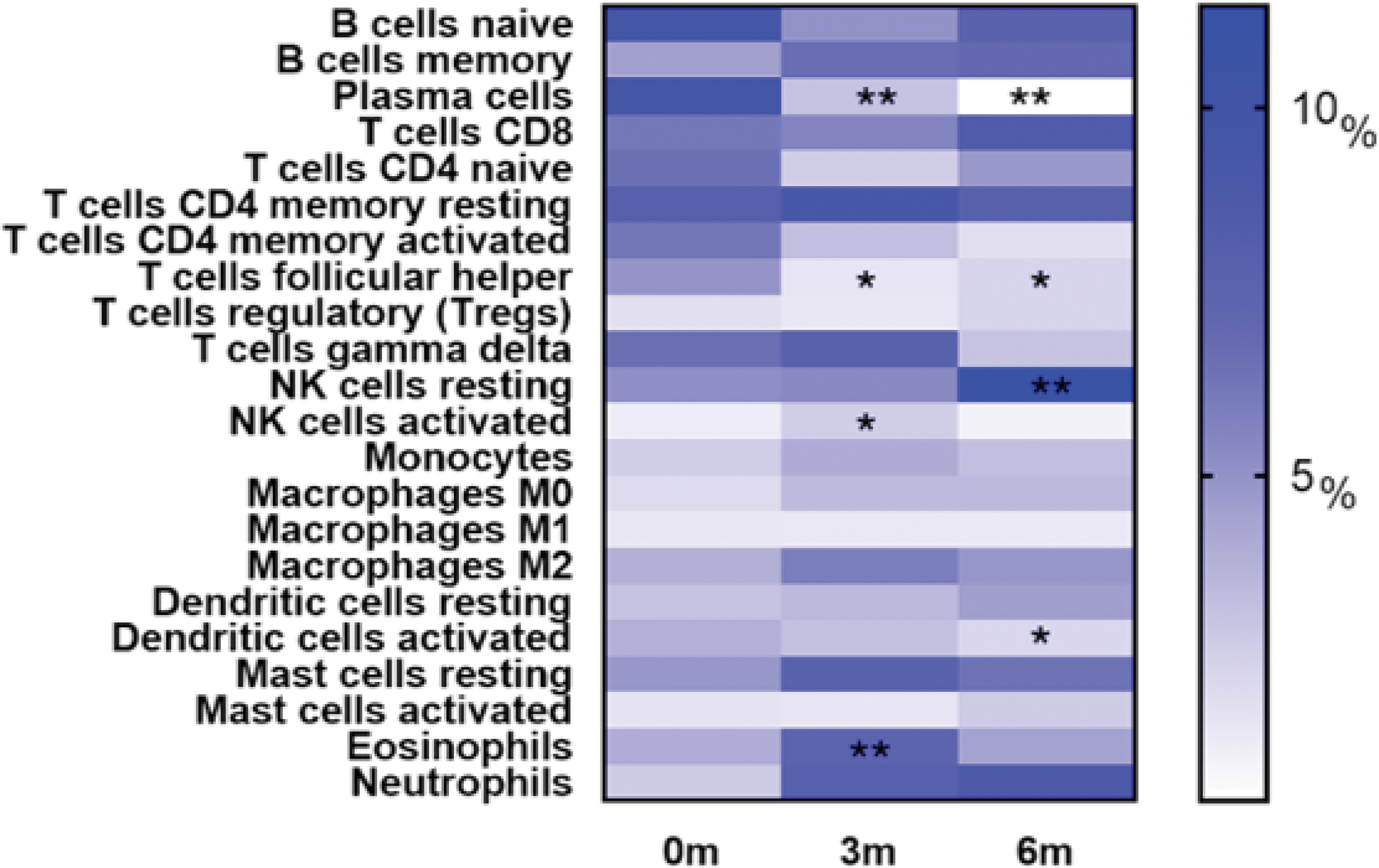
Results: Among the seven screened genes, only ISG15 showed a significant decrease in expression at 6 months (6m) compared to baseline (0m) (p = 0.046), while no significant changes were observed for other genes (Figure 1A). Significant decreases in immune cell proportions were observed over time. Plasma cells and follicular helper T cells decreased at both 3 months (3m) and 6m (p < 0.05). Resting NK cells decreased at 6m, active NK cells at 3m, and activated dendritic cells at 6m (p < 0.05). Eosinophils also showed a significant reduction at 3m (p = 0.002, Figure 2). SLEDAI scores significantly decreased at both 3m and 6m compared to baseline (p < 0.001), indicating reduced disease activity over time (Figure 1B).
Changes in Gene Expression and Disease Activity Over Time. (A) Mean changes in gene expression levels (MFI) for the seven screened genes ( IFI44, IFI44L, IFI27, ISG15, MX1, OAS3 , and RSAD2 ) at 3 months (3m) and 6 months (6m) compared to baseline levels at 0 months (0m). (B) Changes in SLEDAI scores over time, showing baseline (0m), 3m, and 6m measurements. Statistical analysis was performed comparing values at 3m and 6m with baseline (0m) using appropriate tests. Significance is indicated by asterisks: *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001. Error bars represent standard deviations.
Percentages of immune cell populations in peripheral blood at 0 months (0m), 3 months (3m), and 6 months (6m) after treatment with interferon α kinoid. Statistical analysis was conducted comparing immune cell proportions at 3m and 6m to baseline levels (0m) using appropriate statistical tests. Significant changes are indicated by asterisks: p < 0.05 (*), p < 0.01 (**), p < 0.001 (*** ), and p < 0.0001 (***). The color gradient represents the relative percentage of each immune cell type, with darker shades indicating higher proportions.
Conclusion: The present study highlights the effects of interferon α kinoid treatment on lupus nephritis by demonstrating significant reductions in plasma cell proportions and disease activity over time, as reflected by decreased SLEDAI scores. While only ISG15 showed a significant decrease in gene expression at 6 months, changes in immune cell populations further support the immunomodulatory effects of the treatment. However, limitations such as the small sample size, lack of clinical data, and the secondary nature of the analysis warrant further research to validate these findings and explore their implications in different disease states and treatment contexts.
REFERENCES: [1] Almaani, S., Meara, A., & Rovin, B. H. (2017). Update on lupus nephritis.
Clinical Journal of the American Society of Nephrology, 12
(5), 825-835.
[2] Anders, H. J., Saxena, R., Zhao, M. H., & Parodis, I. (2020). Lupus nephritis.
Nature Reviews Disease Primers, 6
(1), 7.
[3] Kirou, K. A., Lee, C., George, S., Louca, K., Peterson, M. G., & Crow, M. K. (2005). Activation of the interferon-alpha pathway identifies a subgroup of systemic lupus erythematosus patients with distinct serologic features and active disease.
Arthritis & Rheumatology, 52
(5), 1491-1503.
[4] Lauwerys, B. R., Ducreux, J., Houssiau, F. A., & IFN-K Study Group. (2013). Interferon-α kinoid induces neutralizing anti-IFN-α antibodies in SLE patients.
Annals of the Rheumatic Diseases, 72
(1), 134-140.
Acknowledgements: We’d like to thank the Mexican National Council of Humanities, Science and Technology (CONAHCYT) for providing the academic grant that made this research possible. Grant ID: PCC-2022-320697.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (