

Background: Cartilage wear in knee osteoarthritis (KOA) is partially linked to reduced boundary lubrication and concomitant increased friction of the articular cartilage. Similarly, the meniscus, which has a role not only as a shock absorber and load distributor but also in lubrication and nourishment of the articular cartilage, is also subjected to wear in KOA. This can lead to meniscal lesions and/or tears that can further exacerbate the progression of KOA. MM-II is a dispersion of empty large multilamellar liposomes for intraarticular (IA) injection recently shown to reduce knee pain for up to 26 weeks in a large global clinical study (NCT04506463). MM-II liposomes have been shown ex vivo to coat cartilage under compression load and provide boundary lubrication, as well as to reduce cartilage degeneration in vivo in a rat KOA model.
Objectives: The aim of the current study was to confirm whether the cartilage coating by MM-II seen ex vivo, occurs in vivo in a KOA setting. To that end, we utilized surgically induced KOA models in rats and rabbits.
Methods: Osteoarthritis was induced in New Zealand White female rabbits (n=5) and in Sprague Dawley male rats (n=5) by anterior cruciate ligament transection (ACLT) associated with partial meniscectomy (MNX) on the right knee. Rhodamine-labelled MM-II liposomes (Rh-MM-II) were prepared from dipalmitoylphosphatidylcholine (DPPC), dimyristoylphosphatidylcholine (DMPC) and 1,2-dipalmitoyl-sn-glycero-3-phosphoethanolamine-N-(Lissamine rhodamine B sulfonyl) (ammonium salt). The Rh-MM-II liposomes were delivered 6 or 8 weeks after induction of the pathology by IA injections into both ACLT/MNX and contralateral (CL) knees of the rats or rabbits, respectively. One rat and one rabbit without any surgical or intraarticular intervention were used as a control. Knees were harvested at one- and two-weeks post-injection, fixed, decalcified in Ethylenediaminetetraacetic Acid (EDTA) and then frozen. Cryosections were stained with 4′,6-diamidino-2-phenylindole (DAPI) to visualize cell nuclei while Rh-MM-II were visualized under TRITC filter (550nmEX/580nmEM). When indicated, hematoxylin-eosin saffron (HES) staining was done to visualize general tissue morphology. Animal use was authorized by the local ethics committee of the CRO and the French Ministry for Education and Research.
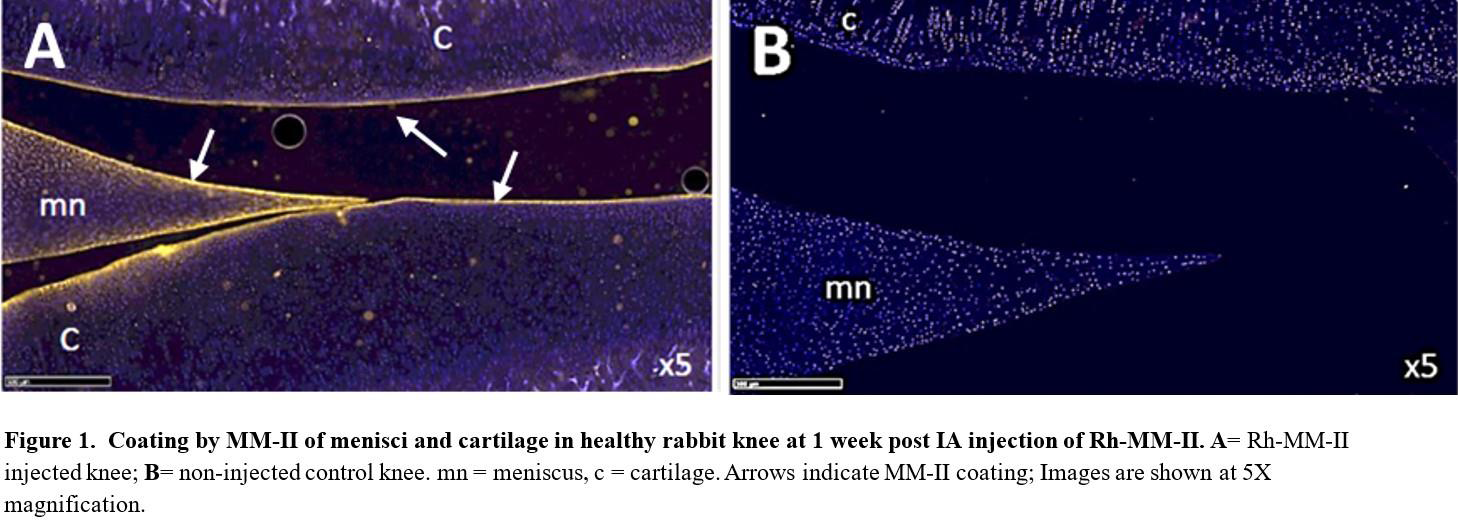
Results: Coating of menisci and tibiofemoral articular cartilage surfaces in both healthy (CL) and ACLT/MNX rat and rabbit knees by MM-II was evident at both one week and two weeks post IA injection of Rh-MM-II. In general, the coating was more pronounced at one week and in healthy knees than at the second week and in ACLT/MNX knees. Fluorescence on surfaces of either the meniscus or cartilage in non-injected control animals was absent, confirming the specificity of the observed signal (Figure 1). In addition to coating of meniscus and cartilage, deposits of MM-II in the synovium were seen in both rats and rabbits, though seemingly larger deposits were seen in the healthy knees compared to the OA knees. These deposits were clearly co-localized with regions exhibiting hypercellularity, most likely of mononuclear cells.
Conclusion: MM-II’s empty large multilamellar liposomes, are reported here to coat both menisci and cartilage for at least 2 weeks in healthy and surgically induced OA knees in two species. Given previously demonstrated research that showed compression to enhance cartilage association of MM-II, the less pronounced coating in OA knees as compared to unoperated knees may be attributed to reduced weight bearing - and hence compression load - on the operated knee. In addition, the synovial localization and the reduced level in OA knees of these liposomes suggest that the liposomes are cleared by recruited mononuclear cells. To the best of our knowledge, an IA-delivered product was rarely, if ever, shown to coat both menisci and cartilage in OA joints. Coating of the menisci is especially intriguing since it is an innervated tissue, and meniscal degenerative tears are associated with progression of symptomatic KOA. The current findings that MM-II coats both meniscus and cartilage with a potentially lubricating layer presents a novel mechanism of action through which MM-II may exert its effect.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Roni Wechsler Received options from Moebius Medical, Current employee of Moebius Medical, Worked as a consultant to Moebius Medical before joining as an employee, Rany Rotem Current employee of Moebius Medical.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (