

Background: Ecto-nucleotidases are membrane proteins that catalyse a sequence of chemical reactions in the extracellular space, leading to the conversion of ATP and NAD+ into adenosine. There are two enzymatic pathways catalysed by ecto-nucleotidases: the so-called “canonical pathway” (CD39 and CD73) and the “non-canonical pathway” (CD38, CD157, CD203a and CD203c). ATP and adenosine are key mediators of the purinergic signaling system, which plays a role in modulating immune system functions. In systemic lupus erythematosus (SLE), increased serum ATP levels and altered leukocyte expression of adenosine receptors suggest a dysfunction in the conversion of purinergic mediators by ecto-nucleotidases. Furthermore, an increase in CD39+ lymphocytes has been observed in SLE patients, while no differences have been described in the expression of other ectoenzymes. However, at the current state, a comprehensive analysis of the expression of these markers has not been conducted.
Objectives: The aim of this study was to characterize the expression of ecto-nucleotidases of the “canonical pathway” (CD39 and CD73) and “non-canonical pathway” (CD38, CD157, CD203a and CD203c) in B and T lymphocytes, NK cells and dendritic cells (DC) from patients with SLE and to evaluate potential correlations with disease activity status.
Methods: Consecutive patients over 18 years old diagnosed with SLE, according to the 2019 EULAR/ACR criteria, and age- and sex-matched healthy controls were included in the study. Blood samples were collected from all participants for the isolation of peripheral blood mononuclear cells, which were analysed using spectral flow cytometry. Ecto-nucleotidases expression was evaluated according to SLE activity status, distinguishing patients in remission—if they met the DORIS definition—from those with active disease. Categorical variables were compared using the χ² test or Fisher’s exact test, when appropriate, while continuous variables were analysed using the t-test or Mann-Whitney test, depending on data distribution. Informed consent was obtained from all participants. The study was conducted in compliance with the principles of the Declaration of Helsinki.
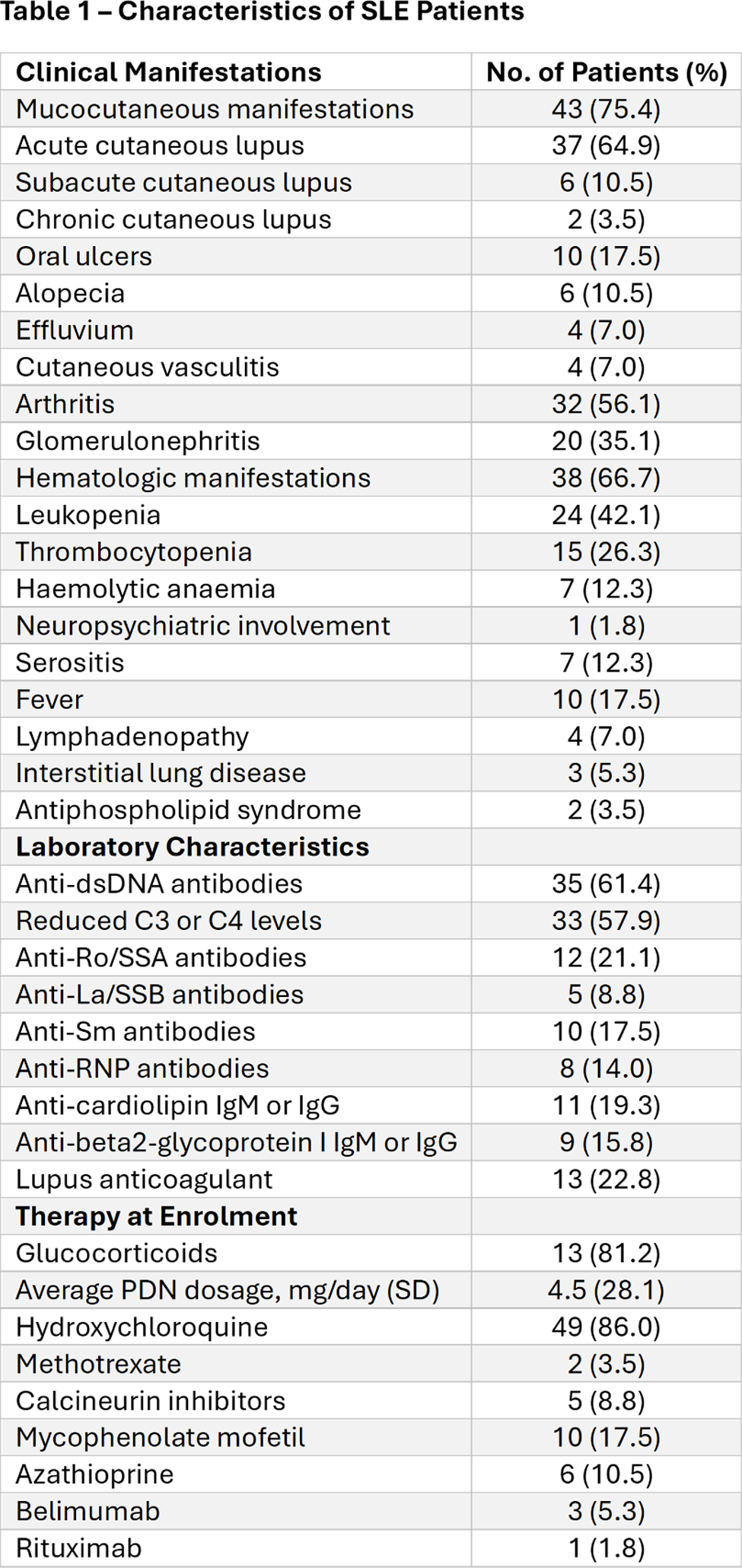
Results: The study included 57 SLE patients, with a female-to-male ratio of 10:1 and a median age at diagnosis of 31 years (Table 1) and 30 healthy individuals matched for sex and age. Compared to controls, patients showed increased levels of CD157+ B lymphocytes (2.38% vs. 1.51%; p=0.031), CD203a+ B lymphocytes (0.89% vs. 0.15%; p<0.001), and CD203c+ B lymphocytes (2.27% vs. 0.17%; p<0.001). In the patient group, there was an increase in CD157+ T lymphocytes (0.65% vs. 0.23%; p<0.001), CD203a+ T lymphocytes (1.37% vs. 0.03%; p<0.001), and CD203c+ T lymphocytes (0.64% vs. 0.07%; p<0.001). Conversely, CD38+ T lymphocytes were reduced in patients compared to controls (60.09% vs. 80.75%; p=0.003). Moreover, an increase in CD73+ (43.14% vs. 31.76%; p=0.004), CD157+ (1.55% vs. 0.54%; p=0.045), and CD203a+ (3.96% vs. 0.05%; p<0.001) Treg cells was observed in patients. Patients also showed higher levels of CD73+ (15.08% vs. 6.72%; p=0.001), CD157+ (7.65% vs. 3.65%; p=0.014), CD203a+ (0.41% vs. 0.02%; p=0.002), and CD203c+ (2.18% vs. 0.10%; p<0.001) myeloid DC cells compared to controls. In NK cells, an increased percentage of CD39+ (1.37% vs. 0.47%; p<0.001), CD73+ (1.73% vs. 0.16%; p<0.001), CD157+ (0.59% vs. 0.13%; p=0.005), CD203a+ (0.14% vs. 0.00%; p<0.001), and CD203c+ (0.43% vs. 0.13%; p=0.001) was observed in patients compared to controls. In the comparison between patients with active disease and those in remission, the percentage of CD203a+ cells was increased in active disease in B lymphocytes (1.32% vs. 0.67%; p=0.027), T lymphocytes (3.05% vs. 2.56%; p=0.006), and NK cells (0.36% vs. 0.10%; p=0.020). Additionally, CD39+ Treg cells were reduced in patients with active disease compared to those in remission (38.62% vs. 61.84%; p=0.027).
Conclusion: In this study, we conducted for the first time a comprehensive analysis of the expression of ecto-nucleotidases in several leucocyte populations in a large cohort of SLE patients. We demonstrated an increased expression of enzymes involved in both the “canonical” and “non-canonical” adenosine pathways in various leukocyte populations. The increased expression of ecto-nucleotidases is known to be driven by hypoxia-inducible factor 1 (HIF1) and several cytokines released during inflammation, such as TGFβ, TNF, IL-2, and IL-6. Interestingly, NK of SLE patients showed an increase of several ecto-nucleosidases, therefore suggesting a potentially regulatory role in the production of immunosuppressive adenosine and depletion of ATP and NAD+. Notably, CD203a expression was higher in B and T lymphocytes and NK cells from patients with active disease. This suggests that CD203a expression might be induced within the pro-inflammatory milieu typical of disease flares and could have regulatory functions in limiting the hyperactivation of the immune system, by degradation of the pro-inflammatory mediators NAD+ and ATP. Of note, reduced expression of CD39 in Treg cells from patients with active disease was observed. Theoretically, this could lead to a localized reduction in ATP levels, potentially impairing the immunosuppressive functions of Treg cells. Therefore, this pathway is of great interest in the identification of targets for immunomodulating therapies. However, further clinical and functional studies are needed to confirm this intriguingly hypothesis. In conclusion, our findings suggest a possible alteration of purinergic mediators regulation in SLE, that could contribute to the pathogenesis of the disease.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (