

Background: Since legalization of medical cannabis (MC) in Canada and some U.S. states for medical and recreational purposes starting from 2001, MC use for pain management has become widespread among patients with rheumatologic conditions throughout North America [1]. However, no data on cannabis use in this patient population are available in Europe. Several European countries permit MC use, still, Germany is the only European country that recently legalized cannabis for recreational use and eased prescription regulations for MC, representing a notable case study for this topic [2].
Objectives: To assess i) the distribution and consumption pattern of cannabis among patients with inflammatory rheumatic diseases in Germany, ii) patient openness to engage in the use of cannabis-based products for pain management, iii) associations of cannabis use with demographic and clinical factors.
Methods: We conducted a prospective observational study on patients with rheumatoid arthritis (RA), spondyloarthritides (SpA), and autoimmune connective tissue disease (CTD). Participants were consecutively enrolled at two centers (University hospital of Erlangen, Charitè Berlin) and completed an anonymous survey approved by the local institutional review board. The questionnaire included 29 questions on demographics (n=2), disease (n=4), ongoing therapies and analgesics use (n=5), pain and efficacy of analgesics and cannabis (n=3), cannabis use (n=6), knowledge and openness to cannabis-based treatments (n=6), drug, smoking status, and alcohol use (n=3). We used chi-square or Fisher’s exact test for categorical variables, Wilcoxon rank-sum or Kruskal-Wallis test for continuous variables, and log-binomial regression to estimate associations between variables. Percentages were calculated on the total of available data for each item.
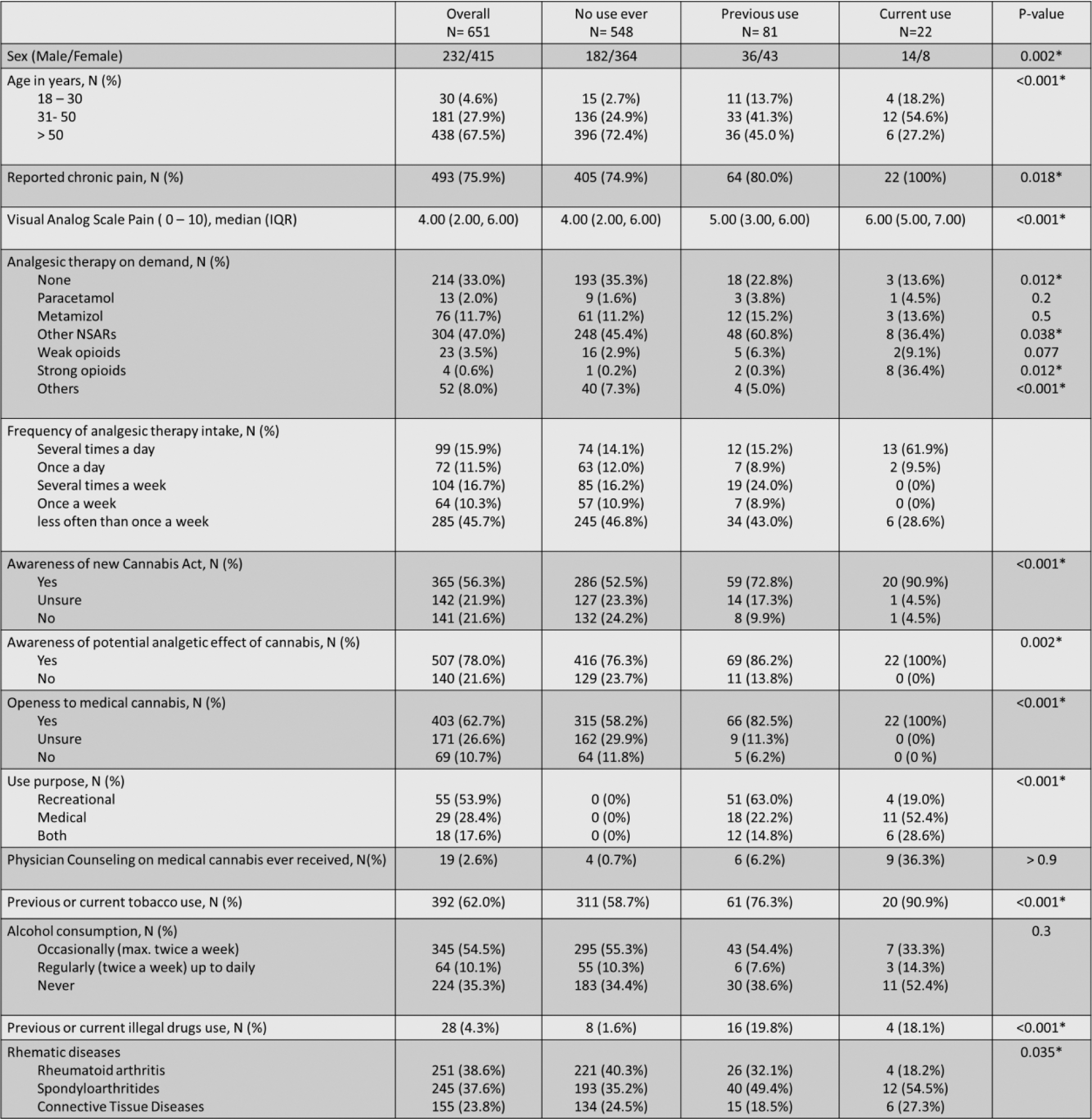
Results: A total of 651 patients were enrolled (n=251 RA, n=245 SpA, n=155 CTD), the majority of whom females (64.3%) and over 50 years old (67.5%) (Table 1). Median (IQR) pain was 4.0 (2.0-6.0) and about one-in-three patients were taking analgesics once or more daily. There was no difference in pain levels and the perceived efficacy of analgesics was equal between diagnosis groups, even if the use of NSAIDs was less frequent in CTD. The large majority (84.2%) declared no history of cannabis use, while previous users were 13.4% and current users were 3.4%. The majority never-users (58%) declared to be open to MC and 30% was unsure, while only a small minority (12%) was opposed. While knowledge on the existence of MC was equal between users and never-users, never-users were reportedly significantly (p<0.001) less informed about the new German law (Table 2). Cannabis consumption was more frequent in males (p<0.001), in individuals under-fifty years of age (p<0.001), and in patients who reported “chronic pain”. SpA patients showed a disproportionately high number of cannabis users (previous or current) compared to RA and CTD (Table 1), with a relative risk (RR) of 1.78 (95%CI 1.18-2.72, p=0.006). However, after adjusting for sex and age, the RR lost its significance. Cannabis users were prescribed more b/tsDMARD and less csDMARD compared to non-users. Use of on-demand analgesics was significantly higher in cannabis users (p=0.012), and particularly opioids. Multiple daily intakes of analgesics were reported in 61.9% of current cannabis users as opposed to 14.1% of non-users. There were no differences in the perception of analgesics efficacy between users and non-users. Active users reported very high median efficacy of cannabis products on pain (8.0 (7.0-10.0)), exceeding that of conventional analgesics (6.0 (4.0-8.0)). Ex-users reported similar median efficacy of cannabis (5.0 (3.0-7.0)) and conventional analgesics (6.0 (4.0-8.0)). Almost half of the cannabis users and more than half of SpA patients declared consuming cannabis for medical purposes. Most users (49.4%) declared to smoke cannabis while the rest mainly resort to oils and edibles. Prescription rates of MC were very low: only 7.1% of users declared a prescription from a physician and the quasi-totality (97.4%) declared to have had no consultation with a physician about MC. Side effects were reported in 32% of active users and 59% of ex-users (Table 2).
Conclusion: Our study shows that German patients with rheumatological diseases use significantly fewer cannabis-based products for pain management compared to North American reports. However, an increase in cannabis use is expected due to (i) relaxed prescription regulations, (ii) the perceived high analgesic efficacy of cannabis, and (iii) strong openness to medical cannabis (MC). Despite these trends, our data reveals significant gaps in the information about MC provided by healthcare professionals. Improved counselling and education from medical providers are essential to support this growing trend and facilitate the legal prescription of cannabis for pain management. Additionally, targeted clinical trials should address the current lack of high-quality evidence on treatment indications and posology to ensure appropriate use in clinical practice [3].
REFERENCES: [1] Boehnke KF, et. al. ACR Open Rheumatol. 2023.
[2] Gesetz zum kontrollierten umgang mit cannabis und zur änderung Weiterer Vorschriften.
Bundesgesetzblatt
. 2024.
[3] Guillouard, M., et al. Rheumatology.
Table 1. Demographic characteristics and data on analgesic therapy.
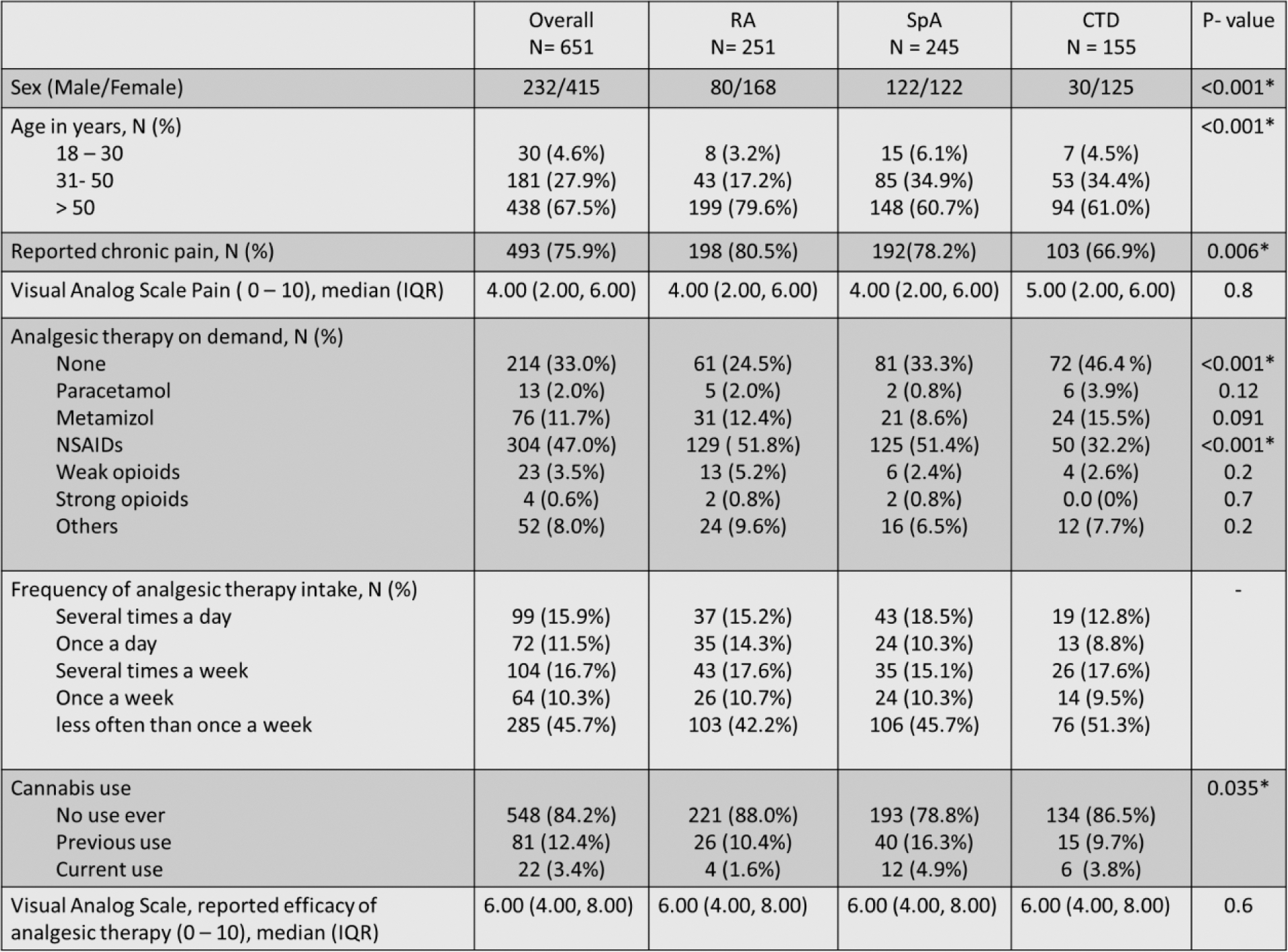
Table 2. Analgesic therapy, attitude towards cannabis, and substance abuse patterns by use of cannabis.
Acknowledgements: NIL.
Disclosure of Interests: Giulia Corte COI not related to this abstract, Koray Tascilar: None declared , Anna Kroker: None declared , Ioanna Minopoulou COI not related to this abstract, Arnd Kleyer COI not related to this abstract, COI not related to this abstract, COI not related to this abstract, David Simon COI not related to this abstract, COI not related to this abstract, COI not related to this abstract, Georg Schett COI not related to this abstract, COI not related to this abstract, COI not related to this abstract, Filippo Fagni COI not related to this abstract, COI not related to this abstract.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (